When kidney damage goes unmanaged it can progress into chronic kidney disease. This condition has 5 stages. All phases of this condition affect the kidneys, however, it is during chronic kidney disease stage 4 that the kidneys become severely impaired. While this is a serious issue there are still things you can do to preserve kidney function. This article is your guide to stage 4 kidney disease. Read on to learn what is stage 4 kidney disease, how to know you have it, how to treat it, and what can be done to prevent it from leading to kidney failure.
Table of Contents
What is Chronic Kidney Disease?
Chronic Kidney Disease (CKD) is a debilitating condition. In CKD the kidneys become damaged and start to lose their function. According to the National Kidney Foundation, thirty-seven million American adults are currently suffering from this condition.
What is Stage 4 Kidney Disease?
Before we discuss chronic kidney disease stage 4 here is some information about kidney disease stages and how the condition progresses.
The disease starts with minor damage to the kidneys. This is known as stage 1. However, when left untreated function will continue to decline. The remaining stages are sometimes referred to as the 4 stages of renal failure.
Stage 2 has a further impact on kidney health but there are no apparent symptoms.
Third stage renal disease is when there are actual physical symptoms that can be determined by a blood test. Stage 3 is the middle point of CKD.
This is when kidney damage has surpassed stages 1 and 2 but there is still a good amount of function left in the kidneys.
(Learn more about stage 3 kidney disease in this article)
Stage 4 kidney disease kicks in when kidney decline has surpassed stage 3. In this stage, there is severe damage done to the kidneys.
Finally, Stage 5 is when kidneys are on their last legs and may result in kidney failure.
What Are the Stages of Kidney Failure?
Kidney disease stages 4 and 5 are often referred to as the kidney failure stages. This is because a good amount of kidney function has been lost.
The disease has passed the middle ground of the third stage. Now the kidneys’ function teeters on the brink of failure.
However, there is still a light at the end of the tunnel, and no, not the bad kind. A silver lining to all of this is that stage four kidney disease is still better than stage 5.
Other names for chronic stage 4 kidney disease include renal failure stage 4 or stage 4 renal failure. These names can be misleading because kidney disease stage 4 the kidneys are still working to some degree.
It is actually during stage five there is little to no kidney function. The kidneys are pretty much done. At this point there is a discussion about dialysis and/or a kidney transplant. This is why stage five is often referred to as end-stage kidney disease (ESKD) or end-stage renal disease (ESRD).
However, kidney stage 4 disease is not as bad as stage 5 it still needs to be taken seriously. Know there is still a lot you can do to preserve kidney function and prevent your body from progressing into the renal failure stage.
What Causes Stage 4 Kidney Disease To Occur?
Like the other kidney disease stages, 4 stage CKD does not just appear one day. Instead, stage 4 kidney disease occurs over time. It is the result of poor kidney function due to chronic kidney disease that goes untreated.
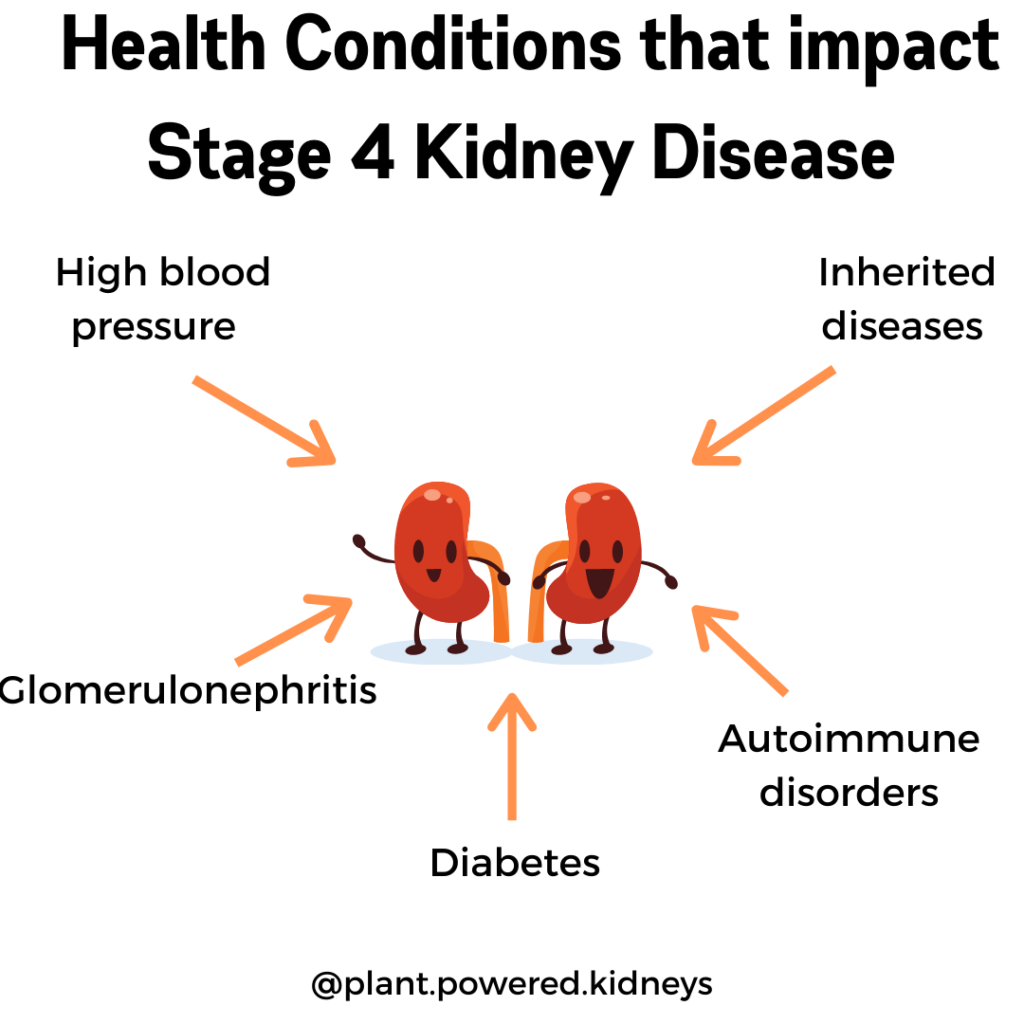
Health Conditions that Impact Stage 4 Kidney Disease
The causes of kidney disease mainly stem from health conditions that cause damage to the kidneys. The longer these conditions go unmanaged the more likely someone will wind up with stage 4 kidney disease. These diseases include:
- Diabetes
- High blood pressure
- Glomerulonephritis
- Inherited diseases
- Autoimmune disorders
Diabetes
Diabetes occurs when your blood sugar gets too high. If left unmanaged it can wreak havoc on the kidney’s blood vessels. Consequently, damaged blood vessels will result in kidneys not being able to work properly.
High Blood Pressure
Blood pressure is regulated by the kidneys. When your blood pressure gets too high it can affect the kidneys. Continuous elevated blood pressure will threaten the health of the kidneys. The kidneys will no longer properly excrete wastes.
Wastes that build-up will cause fluid imbalances further elevating blood pressure. This hypertension also damages blood vessels found in the kidneys and more water retention will ensue.
Glomerulonephritis
Glomerulonephritis is when the kidney’ filtration system becomes inflamed. Inflammation will injure this particular area of the kidneys. Rampant inflammation will further weaken kidney function. It is the third-largest cause of kidney disease.
Inherited Diseases
Unfortunately, some people are born with diseases that can weaken kidney function. These include the following conditions:
- Polycystic kidney disease
- Alport syndrome
- Tuberous sclerosis
- Von Hippel Lindau disease
- Thin Basement Membrane Disease
- Gitelman and Bartter Syndromes
- Lowe Syndrome
- Hereditary Interstitial Kidney Disease
- Fabry Disease
- Nephronophthisis
- Nephrogenic diabetes insipidus
Autoimmune Conditions
An autoimmune condition is when the body attacks its own cells and tissues. This is because the body sees them as a threat. As a result, cells are destroyed and inflammation levels increase. Two autoimmune disorders that can weaken the kidneys are
How is Stage 4 Kidney Disease Diagnosed?
The ultimate guide to stage 3 kidney disease talked about how CKD can go clinically undetected until stage 3. In this stage, a blood and urine test will tell how well the kidneys are working. The same is said for stage 4 kidney disease.
What Measures Kidney Function?
All of the kidney disease stages are measured by a lab value called creatinine clearance. It tells how much creatinine is excreted by the kidneys into the urine.
Creatinine is a waste that is produced from the everyday wear and tear of the muscles.
Since the kidneys are responsible for eliminating wastes, the creatinine clearance can indicate the health of the kidneys.
Estimated Glomerular Filtration Rate (eGFR) Indicates Each of the 5 Stages of Kidney Disease
If you are wondering where your kidney function lies you can also look at your estimated glomerular filtration rate (eGFR). This value is another name for the creatinine clearance mentioned above. It is a more accurate indication of kidney function.
eGFR includes the following:
- Creatinine clearance
- Age
- Body size
- Gender
It is calculated by your doctor to determine your specific eGFR. The worse the kidney function, the lower the number. See below for the eGFR for each of the 5 stages of kidney disease.
CKD Stage Chart
| CKD Stages | eGFR range | Notes |
|---|---|---|
| – Stage 1 | 90 mL/min or higher | During stage 1 there is some damage to the kidneys, but their function is still normal. There is about 90 to 100 percent of kidney function during CKD stage 1. This stage has kidney damage with normal kidney function. |
| – Stage 2 | between 60 and 89 mL/min | In CKD stage 2 the kidneys are damaged but still have only a mild loss of function. Usually, they have 60 to 89 percent of function left. |
| – Stage 3a | between 45 and 59 mL/min | The CKD Stage 3A has mild to moderate loss of kidney function. Now the kidneys are functioning between 45 to 59 percent capacity. |
| – Stage 3b | between 30 and 40 mL/min | The CKD 3B stage of kidney disease has moderate to a severe loss of kidney function. The kidneys have only 30 to 40% function left. |
| – Stage 4 | between 15 and 29 mL/min | In CKD stage 4, there is severe loss of kidney function. |
| – Stage 5 / ESRD | less than 15 mL/min | CKD stage 5 is when kidney failure or end-stage renal disease (ESRD) sets in. So there is less than 15% of kidney function available. This stage can require dialysis or a kidney transplant. |
Risk factors
There are a few risk factors that increase the chances of CKD progressing to stage 4 kidney disease. These include risk factors from underlying conditions.
Also, risk factors exist that you may or may not be able to control.
Risk Factors From Underlying Conditions
Controlling risk factors from underlying conditions can prevent stage 4 kidney disease from moving into stage five. These include the following:
- Diabetes
- Managing existing hypertension
- Autoimmune disorders
- High cholesterol
- Atherosclerosis
- Kidney stones
- Urinary Tract Infections (UTIs)
- Enlarged prostate
- Obesity
- A genetic disorder that produces cysts in and/or damages the kidneys
- A kidney infection
- Scleroderma
- Liver disease
- A drug that is toxic to the kidneys
- Conditions that inflame the kidney
- Heavy metal poisoning (lead poisoning)
- Conditions that damage blood vessels in the kidneys (hemolytic uremic syndrome)
- Conditions that damage arteries in the kidneys (renal artery stenosis)
- Obstructive sleep apnea
Risk Factors You Cannot Control
Some risks you cannot change. These include
- Genetics
- Family history of CKD
- Family history of kidney failure
- Age
- Gender
- Your low birth weight
- Race
- Ethnicity
This is why a higher prevalence of CKD occurs among African Americans, Hispanics, Native Americans, Asian Americans, and Pacific Islanders. These groups of people also have a greater risk of diabetes and heart disease. When co-existing conditions go uncontrolled kidney function will suffer and there is a likely chance that stage 4 kidney disease will occur.
Risk Factors You Can Control
You may be thinking a lot is working against you. Don’t worry! There is still a lot you can do to control CKD from moving past stage 4. They include the following:
There is also a lot you can do with these. Just a few lifestyle changes can prevent further progression of stage 4 kidney disease, but you can read more on that later!
CKD Stage 4 Symptoms
In the early stages of CKD, there are no symptoms so it’s hard to tell anything is even happening. This can be problematic because you may have no idea your kidney function is declining.
By the time stage 4 kidney disease takes place, there are tell-tale signs that something is wrong with your kidney function.
CKD stage 4 kidney disease symptoms include the following:
- Swelling in the hands and feet
- Back pain
- Weakness
- Poor mobility
- Poor appetite
- Little energy and fatigue
- Itching
- Difficulty breathing
- Trouble sleeping
- Bone or joint pain
- Changes in urination
- Color changes in urine (red, dark orange, brown)
- Foamy urine
- Bad Breath
- Weird taste in the mouth
- Poor concentration
Complications
Alternatively, if your kidney disease and/or pre-existing health conditions are not dealt with, kidney function will continue to decline. This will become a big problem and what results is that the kidneys will no longer be able to remove wastes. The next thing you know wastes are starting to build up in the body. This will lead to a ton of health complications including
- High blood pressure
- Reduced red blood cell count (anemia)
- CKD Mineral and Bone Disorder (MBD)
- Heart disease
- Diabetes
- Nutritional changes
- Neurological problems
- Elevated cholesterol
- Hardening of the Arteries
- Electrolyte imbalances
- Toxin build up in the blood
- Increased acid production
High Blood Pressure
Hypertension and high blood pressure can occur during any stage of CKD and is prevalent during stage 4. This condition increases the pressure of blood flow through the veins. It puts pressure on blood vessels found in the kidneys.
This will cause damage to the blood vessels. Injury to the blood vessels can impair the kidneys’ ability to remove fluid and wastes from the body. An increase in fluid leads to an increase in blood pressure.
This vicious cycle of high blood pressure, blood vessel damage, and decline in kidney function will put the body on the path of kidney failure unless hypertension is treated.
Hypertension also puts you at a higher risk of getting heart disease. Uncontrolled blood pressure also increases the risk of death.
Reduction in Red Blood Cells (Anemia)
Having too few red blood cells is also a problem that arises from unmanaged kidney disease. Known as anemia, this condition has many root causes. However, most times those with CKD, have it due to a lack of erythropoietin.
This hormone helps make red blood cells. It is released by the kidneys so when the kidneys are in bad shape there will be a decrease in the production of erythropoietin. The only problem is that the less of this hormone means the more likely someone will have not enough red blood cells and will develop anemia.
If left untreated anemia can lead to heart disease. Red blood cells are needed to deliver oxygen to the brain so a decrease in these cells can also affect brain function and increase the risk of stroke in those with CKD.
CKD Mineral and Bone Disorder (MBD)
Kidney dysfunction affects how minerals are metabolized. Therefore, CKD Mineral and Bone Disorder (MBD) will result. This condition occurs throughout all stages of CKD and causes abnormalities in
- Calcium metabolism
- Phosphorus metabolism
- Parathyroid hormone (PTH) metabolism
- Vitamin D metabolism
- Bone metabolism
- Vascular or other soft tissue calcification
The kidneys are responsible for metabolizing minerals. So poor kidney function leads to MBD and changes body levels of phosphorus, calcium, and vitamin D.
During stage 4 kidney disease calcium and phosphorus levels are also altered resulting in low levels of calcium (hypocalcemia) and high levels of phosphorus (hyperphosphatemia). This is because weakened kidneys are not able to remove phosphorus from the blood.
To preserve low calcium levels the body will tell the brain to secrete parathyroid hormone. This hormone makes the kidney stop removing calcium from the body.
The secretion of PTH also induces secondary hyperparathyroidism. This condition removes calcium from the bones to correct hypocalcemia. It is also another reason why bone loss occurs in CKD
Kidney dysfunction also prevents the kidneys from being able to make the active form of vitamin D.
All of these actions will affect bone metabolism and lead to weakened bones.
Hardening of arteries in the kidneys also occurs in stage 4 CKD. This vascular calcification may be due to MBD. This serious condition can lead to heart disease.
Heart disease
Even having just mild to moderate kidney problems can increase cardiovascular risk. About 50 percent of people with CKD stage 4 have cardiovascular disease (CVD). Heart disease also accounts for about 40 to 50% of the deaths in CKD.
Having diabetes also increases your chances of getting heart disease.
Diabetes
Unmanaged diabetes can weaken your kidneys and cause chronic kidney disease. Having CKD alone can also lead to diabetes.
Weak kidneys cannot remove urea, a waste product from the blood. Too much urea can cause inflammation. It also may prevent insulin from being produced. Less insulin means blood sugar will not be able to get into cells.
Instead, the insulin will stay in the blood, elevating blood sugar. Continuous high levels of blood sugar will lead to diabetes.
So if blood sugar is not controlled those with CKD are at risk for developing diabetes and those with uncontrolled diabetes are susceptible to getting stage 4 kidney disease.
Nutritional Changes
During kidney disease, the digestion and absorption of nutrients are altered. This can lead to changes in the needs of
- Protein
- Water
- Salt
- Phosphorus
If not monitored malnutrition could occur. The risk of folate, iron, and pantothenic acid vitamin deficiencies is common in CKD.
Excess waste products are also a side effect of altered metabolism. Too much uremia can prevent the body from producing energy no matter what is their intake of protein and carbs. This is another form of malnutrition known as uremic malnutrition.
If nutritional issues are left untreated it can lead to anemia, heart disease, and metabolic imbalances.
Neurological Problems
Kidney problems and coexisting conditions like hypertension and diabetes that are not improved can lead to neurological problems like nerve damage and poor cognitive function.
Nerves are needed to bring messages between your brain and other body parts. Damaged nerves will cause peripheral neuropathy, a numbness or tingling sensation in the hands and feet. Nerves get damaged due to
- High blood sugar
- Elevated PTH
- Electrolyte Imbalances
- High uremia levels
- Inflammatory compounds glycotoxins or advanced glycation end products AGE’s in
AGE’s are found in processed foods and also a by-product of digestion. An accumulation of them can result in nerve damage. These are also found in non-diabetics.
Neurological conditions can also slow digestion. This leads to indigestion and other digestive problems.
People with CKD are more prone to having neurological problems when kidney disease and its associated complications go untreated.
Elevated Cholesterol
Higher total cholesterol is associated with low eGFR and weak kidney function are. The “good” HDL cholesterol is also reduced in those with poor kidney function. So improving cholesterol levels may help manage CKD.
Hardening of the Arteries and Plaque Build-Up (Atherosclerosis)
Just like your arteries, blood vessels in the kidney are at risk for atherosclerosis. When there is damage to a kidney blood vessel the immune system will work to heal the wound. This causes plaque and hardening of kidney arteries.
Patients with both early and later stages of kidney disease were found to have atherosclerotic lesions.
Those with moderate to severe impairment of kidney function (stages 3, 4, and 5) are associated with accelerated atherosclerosis. Having an eGFR less than 60 mL/minute puts you at a greater risk for the development of CVD.
See risk other factors for atherosclerosis in this post.
Electrolyte Imbalances
When the kidneys are not functioning, fluid and electrolyte levels get all messed up. These minerals are responsible for regulating acid balance, along with nerve and muscle function. They consist of
A common problem in stage 4 is too much potassium in the blood. Sodium imbalances will also occur when the kidneys cannot regulate fluid levels. Changes in fluids can cause swelling, hypertension, and CVD.
Changes in the levels of the minerals are also responsible for
Toxin Build Up In the Blood (Uremia)
When the kidneys don’t work right, the blood will fill up with toxins like urine. This condition is known as uremia. It can start happening as early as stage 3 so you may have already been suffering from this condition and not realize it.
Learn what symptoms indicate you’re suffering from uremia in this post.
Uremia causes nerve and brain damage. Its effects can cause loss of feeling in the extremities. It is the culprit that forms toxic compounds in the brain as well as a precursor for inflammation and arterial damage.
Increased Acid Production
Poor working kidneys cannot clear acid from the body. High levels of acid lead to metabolic acidosis.
Metabolic acidosis is a major health concern for those with CKD. It has serious health consequences affecting muscle, hormone, and bone function.
Can Stage 4 Kidney Disease Get Better?
Many people wonder if there is anything they can do about chronic kidney disease. They often ask “can you reverse stage 4 kidney failure?” or “can kidney disease get better?”
Unfortunately, reversal is not an option. By this stage, there is a severe loss of kidney function. However, there is still a beacon of hope for your kidneys even at this late stage in the game.
While you cannot repair the damage that has been done to your kidneys, you can delay kidney failure by preventing the progression of CKD.
So if you’re looking to preserve kidney function you should seek help from medical and nutritional professionals skilled in this area of health. They will put together a special care plan to help stop disease progression.
When Should You See a Kidney Doctor?
A kidney doctor is known as a nephrologist. These healthcare professionals are experts in renal health. They provide medical advice as well as diagnose, treat and manage kidney problems and CKD.
A nephrologist is often referred by your primary medical doctor when your labs indicate kidney health may be compromised.
People who do not have kidney issues should see a kidney specialist when they have the following signs and symptoms:
- Get a lot of urinary tract infections (UTIs)
- Recurring kidney stones
- Foamy urine
- Itchy Skin and Joint or Bone Pain
- Tiredness
- Insomnia
- Changes in urination
- Family history of kidney problems and kidney disease
- High blood pressure
- Diabetes
- Heart disease
- An inherited condition that leads to kidney disease
- A lot of blood in the urine
- A lot of protein in the urine
- Recurring kidney stones
People in stage 4 CKD are typically seeing this doctor at least every three months. They will monitor labs and manage any underlying conditions you may also have.
If you have not yet seen a kidney doctor your primary doctor and/or insurance company can refer you to a local nephrologist.
When Should You See a Renal Dietitian?
Like nephrologists, a renal dietitian (RD) is a specialist in renal nutrition. These professionals should be part of your healthcare team. They can help you with the nutritional aspect of kidney disease. They diagnose and assess the nutritional problems that may arise from CKD.
Renal dietitians create specific individualized meal plans to improve their kidney health.
They also help improve nutrition status to
- Increase eGFR
- Manage a healthy weight
- Find healthy food that tastes good
- Make like with CKD 4 more enjoyable
- Find realistic solutions
- Individualized meal plans that improve nutritional status
- Reduced acid production
- Eat without restrictions
They will educate you on how to preserve kidney function and stop CKD from moving into stage five.
You can find a skilled renal RD through your health insurance provider. You can also find one in the National Kidney Foundations’ dietitian directory.
If you are not living in the states you can check out these international dietetic associations to find renal RDs in countries around the world.
Treatment for Stage 4 Kidney Disease
Though kidney disease cannot be reversed there is still a lot that can be done to preserve the remaining kidney function. So if you haven’t already implemented a treatment plan you need to do this ASAP.
This means finding a kidney doctor and renal dietitian who can implement a kidney care plan that will work to improve your health.
Typically kidney disease treatment consists of medical, nutritional, and lifestyle interventions.
Both your primary care and kidney doctor will be responsible for medical treatments. Your renal RD will work on a plan to improve any nutrition issues. Lifestyle interventions may be mediated by both your doctor and dietitian.
Medical Treatment for Stage 4 Kidney Disease
Medical treatment for stage 4 kidney disease will often consist of medications that are prescribed to manage co-existing conditions. These often include diabetes and blood pressure medications.
There can also be restrictions on certain medications when someone’s eGFR is less than 60 mL/min. Some medicines may harm kidney function. These include
- Cefepime
- Pethidine
- Lithium
- Glibenclamide
- Metformin
- Spironolactone
- Methotrexate
- Enoxaparin
- Diclofenac
- Ibuprofen
- Indomethacin
- Other nonsteroidal anti-inflammatory drugs (NSAIDs)
- Selective COX-2 inhibitors
Gadolinium preparations in magnetic resonance imaging (MRI) dye cause a condition called nephrogenic systemic fibrosis (NSF). NSF causes hardening of the skin and kidneys.
People with an eGFR of less than 30 mL/minute are at risk for this condition and gadolinium should be eliminated from the body with hemodialysis if there is gadolinium in the MRI.
Doses of certain medications may also be tweaked to prevent further kidney dysfunction when the eGFR is below 60.
If you are concerned about your kidney function, ask your doctor about possible medication restrictions.
Does Stage 4 Kidney Disease Require Dialysis?
You may be wondering, does stage 4 kidney disease require dialysis? You will be happy to know that no, dialysis is not needed at this stage of the disease.
It is important to note, however, that there is still severe kidney damage that has occurred. So in regards to how long can a person live with stage 4 kidney failure without dialysis depends on the current and future health of the kidneys.
Now is the time to do whatever you can to preserve the life of the kidneys. This means managing comorbidities like hypertension, heart disease, diabetes, anemia, and other complications that may arise.
Stage 4 kidney disease is often the time when a nephrologist will discuss the possible future need for a kidney transplant.
Stage 4 Kidney Disease That Goes Unmanaged May Need Dialysis
If you are not careful, the disease could move to stage 5 kidney failure. At this point, you will need dialysis to continue to live unless you can get a new kidney.
There are two forms of dialysis:
- Hemodialysis
- Peritoneal dialysis
Hemodialysis (HD) is a treatment that replaces the function of the kidneys. It removes wastes and extra fluid from your blood. When dialysis is done in the privacy of your own home it is called home dialysis.
You can also have HD done at a dialysis center. Treatment runs three to five times a week. Times vary depending on where it is done. It can run one and a half to two hours at home or three to five hours in a center.
Peritoneal dialysis (PD) is an at-home dialysis treatment that must be done daily. It requires minor surgery to place a catheter in the abdomen. In this form of dialysis, the blood is cleaned inside the body.
A cleansing solution known as the dialysate flows into the belly through a tube called the PD catheter. The lining of the stomach or peritoneum is what filters the blood.
Wastes and extra fluid pass through the belly. They need to be drained and replaced with a new dialysate after about a half-hour.
Lifestyle Treatment for Stage 4 Kidney Disease
Additional treatment for stage 4 kidney disease included lifestyle changes. These can be part of both your medical and nutritional interventions. They include:
- Increase daily exercise
- Stress and anxiety management
- Become a nonsmoker
- Improve sleep heath
Increase Daily Exercise
Exercise is important for kidney health. For those with CKD exercise should be approached with caution. Too little or too much intense exercise could be problematic for people with this condition.
It is important to get moving and be active no matter what stage of CKD you have. Types of exercises you can incorporate include
- Aerobic exercises (walking, running, biking, rowing, dancing, elliptical training)
- Weight lifting (squats, push-ups, sit-ups, resistance bands, and free weights)
- Balance exercises
- Stretching (yoga, pilates)
Aerobic exercises will improve heart function and lower blood pressure.
Weight lifting will build muscle which can help manage blood sugar.
Balance exercises will help to prevent falls.
Implementing stretching will improve your muscle strength and overall health.
If you are not already exercising, it is best to talk to your doctor or kidney specialist. They will help you find an exercise plan that is easy to incorporate into your daily routine.
It is also important to note that some people with CKD may have limitations with their exercise. You should not exercise if
- You feel sick
- Your doctor told you not to exercise
- Your body feels tired and needs to rest
Learn more about exercise for kidney health in this post.
Stress Management
Unmanaged stress and anxiety can weaken your kidneys. Even just having a lot on your plate can cause the body to become stressed out. Mellow out with these activities:
- Exercise
- Get a pet companion or look at pictures of animals
- Nourish our bodies
- Limit caffeine intake
- Deep breathing
- Meditation
- Gratitude practices
Learn more about how to manage chronic stress in this post.
Become A Nonsmoker
Smoking is one of the worst things for kidney health. It can
- Slow blood flow to kidneys
- Weak kidneys
- Cause CKD
- Make CKD worse
Smoking increases the risk for stroke and heart attacks in those with high blood pressure. Smoking can also interfere with some hypertension medications.
For anyone with diabetes, smoking may worsen heart, blood vessels, and result in poor wound healing.
Second-hand smoke is just as bad and can lead to similar health problems.
If you need help quitting smoking, talk to your healthcare team.
Improve Sleep Health
According to research, kidney function is regulated by the sleep-wake cycle. People with poor sleep habits will have a faster decline in kidney health.
Be sure to make time for sleep. Try to get between 7 and 8 hours of sleep each night. Here are some tips to improve bedtime behaviors
- Get up and go to bed at the same time every day, even on the weekends
- Avoid alcohol before bed
- Wind down an hour before bed without any artificial lights from TV and other screens
- Avoid heavy/large meals within a few hours before bed
- Stop using caffeine, nicotine, and other stimulants
- Try to spend time outdoors daily
- Have a quiet, cool, and dark bedroom
- Take a hot bath or use stress management techniques before bed
If you still have trouble sleeping, talk to your nephrologist and renal dietitian about what else you can do to improve sleep health.
Additional Lifestyle Recommendations
There are additional lifestyle recommendations that include
- Keeping a healthy weight
- Limiting alcohol
- Reducing hypertension
- Regulate blood sugar
We will discuss them in detail in the nutritional treatment section below.
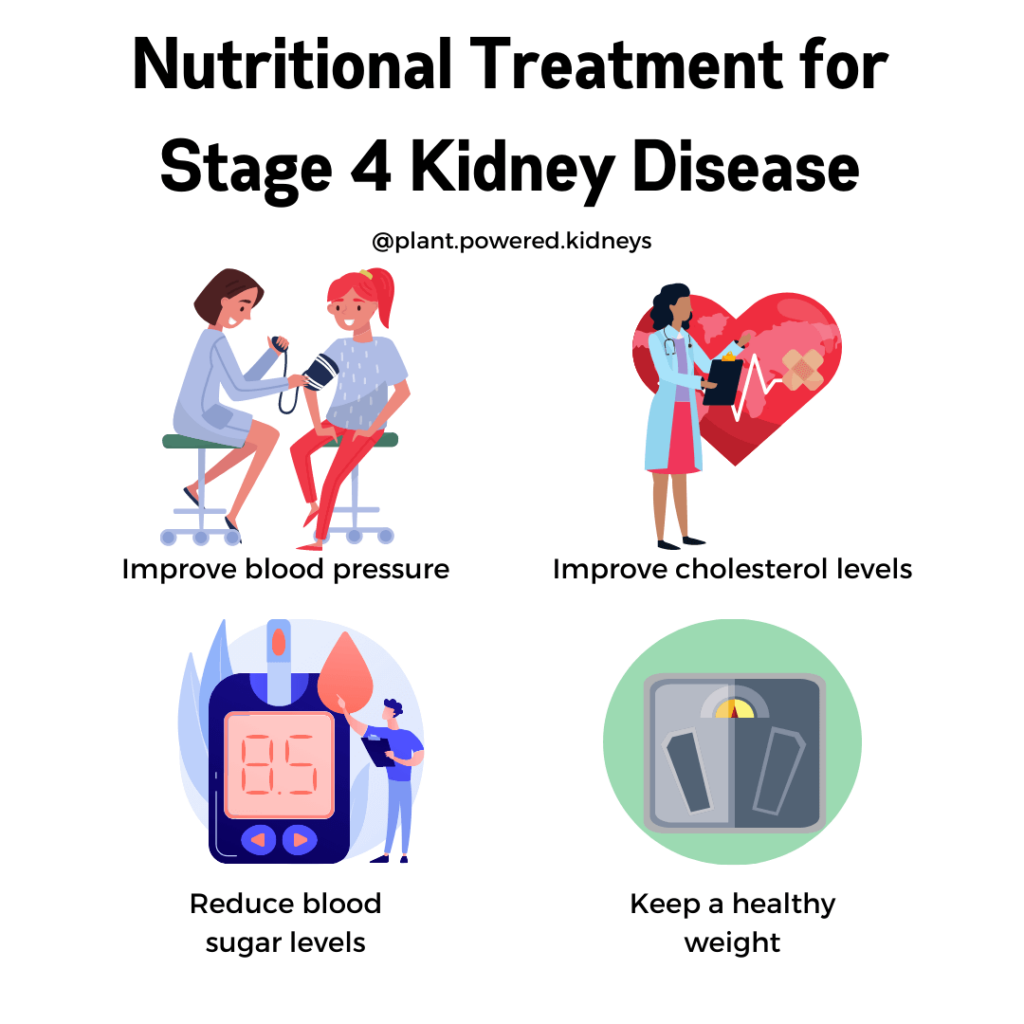
Nutritional Treatment for Stage 4 Kidney Disease
The nutritional treatment for stage 4 kidney disease is all about improving diet to improve co-existing conditions and complications. The hope is to
- Improve blood pressure
- Improve cholesterol levels
- Reduce blood sugar levels
- Keep a healthy weight
This section will outline all that is needed to enhance nutrition status so stage 4 will not turn into kidney failure. It will go over
- Nutrition to manage existing health conditions
- Labs that indicate kidney function
- Nutrients that indicate kidney function
- Foods that will induce kidney damage
- Foods that can help kidney function
We will also provide you with a sample stage 4 renal diet menu plan.
Manage Pre-Existing Conditions and Complications
Good nutrition is so helpful in managing complications and conditions that occur in CKD. In this section, we will tell you everything you need to do nutritionally to improve
- High blood pressure
- Anemia
- MBD
- Diabetes
- Nutritional challenges
- Neurological problems
- Elevated cholesterol
- Hardening of the arteries
- Electrolyte imbalances
- Toxin build up in the blood
- Increased acid production
- Heart disease
High Blood Pressure Nutrition Interventions
When you have high blood pressure the easiest thing you can do is to cut back your sodium intake. Weakened kidneys are not able to excrete sodium properly so having less salt in the diet will help prevent further damage.
Current sodium recommendations are 2,000 mg a day. Those with hypertension should drop their intake down to around 1,500 mg according to the American Heart Association.
However, if your medical team has a different number it is best to follow their direction.
Look for low-sodium snacks and implement The Dietary Approaches to Stop Hypertension (DASH) diet as a way to decrease your sodium intake. This food plan is made up of fruits, vegetables, low-fat dairy, whole grains, fish, poultry, dry beans, seeds, and nuts.
So you will get less sodium and sugar and more of the good stuff your body needs like fiber and lean protein.
When in doubt, stick to a higher intake of whole fruits and vegetables and low to no sodium added snacks like the ones in this post.
Nutrition Interventions for Inadequate Red Blood Cell Count (Anemia)
When your anemia is corrected your body will produce more red blood cells. This means more energy to do the things you want to do!
While getting more blood will increase red blood cell production there is something you can do nutritionally to improve anemia. That is eating more iron-rich foods.
Iron is found in both animal and plant sources. These include
- Lean beef
- Lentils
- Leafy greens
- Mushrooms
- Chickpeas
- Tofu
- Flaxseed
- Olives
- Oats
- Quinoa
With plant foods, you can up the absorption rate by eating them with a food that contains vitamin C like bell peppers, strawberries, broccoli, chili peppers, thyme, kale, and/or citrus.
Certain minerals reduce your iron absorption so don’t eat iron-rich foods with the following:
- Dairy foods
- Tannins (coffee and tea)
- Phytates (grains, legumes, nuts seeds)
Aside from foods, the use of a cast-iron pan in your cooking will amp up your iron intake by as much as 16 percent.
If food and cast iron do not improve your red blood cell count you may need a supplement. Talk to your kidney specialist and renal RD to find out what is right for you.
CKD Mineral and Bone Disorder (MBD) Nutrition Interventions
During stage 4 kidney disease, CKD Mineral and Bone Disorder (MBD) will make your vitamin D, calcium, and phosphorus levels get out of whack.
Decreases in calcium and vitamin D are just as dangerous as the elevations that occur to serum phosphorus levels.
Like in other stages of CKD, treatment involves regulating these nutrients along with the PTH levels if necessary.
How to Regulate Phosphorus Levels in Stage 4 Kidney Disease
Foods with phosphorus may need to be limited. Many processed foods contain phosphorus. It is best to avoid anything with “PHOS” on the food label.
There is also naturally occurring phosphorus in some food and beverages (more information about those below).
Phosphate binder medications are sometimes recommended to get phosphorus levels in check. These are only given if the eGFR is below 50 mL/min.
Learn more about phosphate binders in this post.
Another way to balance out phosphorus is by increasing calcium and vitamin D levels in the blood.
How to Regulate Calcium Levels in Stage 4 Kidney Disease
Calcium levels can be increased by adding calcium-rich foods like dairy (milk, cheese, yogurt, ice cream, leafy greens). Dairy foods are high in phosphorus so if you need to limit this nutrient be careful where you get your calcium.
Excess calcium can also prevent vitamin D from being metabolized. So it’s important to have just the right levels of this mineral.
Calcium supplements may be added to the diet if necessary. They should only be taken under the supervision of your medical team.
How to Regulate Vitamin D Levels in Stage 4 Kidney Disease
Vitamin D can be increased through food, supplements, and the sun. The best food source is fatty fish (salmon, trout, tuna, mackerel, fish liver oil). Some vitamin D can also be found in mushrooms, beef, liver, cheese, and egg yolks.
Depending on your mineral levels some of these foods may need to be limited.
Like calcium, vitamin D may need to be supplemented if your levels are low.
When it comes to phosphate binders, calcium, or vitamin D supplements check with your healthcare team to find out if they are necessary for your health.
Diabetes Nutrition Interventions
We know diabetes is a leading cause of kidney disease so managing this condition will help improve kidney function. Diabetes nutrition interventions include regulating
- Blood sugar levels
- Sodium levels
- Potassium levels
- Phosphorus levels
How to Regulate Blood Sugar in Diabetes-Related to Stage 4 Kidney Disease
Regulating blood sugar and controlling diabetes and CKD can be done mainly through diet. The easiest thing to do is cut back on added sugar and refined carbohydrates. This means less processed foods and more fiber-rich fruits and vegetables.
Fiber can slow digestion so foods with this nutrient will keep you fuller longer. This nutrient does not require insulin to be absorbed so there is less of an insulin response when compared with glucose.
Prebiotics are the byproducts formed when fiber is digested. Healthy bacteria in the gut feed on these substances and will improve gut health.
You also want to focus on low glycemic foods. They will regulate blood sugar by preventing that glucose spike that may occur after mealtimes. The glycemic index is a measure of low glycemic foods.
This rating system looks at how much a particular food will elevate your blood sugar in relation to a piece of white bread that has a glycemic index of 100. Foods with a glycemic index of less than 55 are considered low glycemic foods.
These foods include whole grains like quinoa, oats, and wild rice.
How to Regulate Sodium, Phosphorus and Potassium Levels in Diabetes-Related to Stage 4 Kidney Disease
When you have both diabetes and stage 4 kidney disease you will need to monitor nutrient levels. Particularly, sodium, potassium, and phosphorus levels.
With this stage of CKD come phosphorus and sodium restrictions. These nutrients are added to a lot of processed foods but also occur naturally. So you will need to watch your intake of certain foods and beverages.
See what foods to steer clear of in the “Avoid High Phosphorus Foods” and “Avoid High Sodium Foods” sections below.
Potassium restrictions are also a possibility when you have both diabetes and this stage 4 CKD. See the “Avoid High Potassium Foods” section to know what foods may alter your levels of this vitamin.
Learn more about a renal diabetic diet in this post.
Neurological Problems Nutrition Interventions
Nerve damage, poor brain function, and slowed digestion arise from damage from unmanaged kidney disease.
Nutrition interventions for neurological problems include a diet rich in fruits and vegetables. The antioxidants found in these foods calm the inflammation that may arise from high blood sugar, hypertension, and excess AGE’s.
Getting more fiber and fluids will also improve digestion speed. As with diabetes, regulating blood sugar can prevent neurological conditions caused by damage to nerves.
Restricting potassium may also be necessary to preserve nerve function.
B12 is a nutrient that may improve cognition in those with CKD. Incorporating foods like fish, meat, poultry, eggs, dairy, and fortified nutritional yeast for increased B12. Supplements may sometimes be necessary depending on a person’s current status.
Be sure to ask your dietitian about your nutrient needs before increasing fluid intake or taking any supplements.
Elevated Cholesterol Nutrition Interventions
Though people with CKD may be put on cholesterol medications, improving diet should be the first step to take if you want to lower your cholesterol.
The American Heart Association recommends saturated fat intake be only 10 to 15 grams for a healthy person. Saturated fat intakes higher than this were associated with an increase in total and the “bad” LDL cholesterol.
Saturated fat is found in the following foods:
- Fatty meats
- Pork
- Lamb
- Butter
- Cheese
- Cow’s milk
- Baked goods
- Packaged foods
- Coconut oil
- Palm kernel oil
- Palm oil
- Lard
- Shortening
- Bacon fat
- Cocoa butter
- Butter
- Margarine
So be sure to limit or avoid these items. If you are unsure about the saturated fat content check out the product’s food label to avoid getting any hidden saturated fat.
If you’re having more than one alcoholic beverage a day, it may be too much. Alcohol increases cholesterol so limit your intake. If you’re unsure, check with your doctor and renal RD for specific recommendations.
Fiber is cholesterol’s enemy so eat up this nutrient to get your numbers down. Look to get at least 25 to 35 grams of fiber a day. Eat fruits, vegetables, nuts, seeds, beans, and whole grains to get to your goal.
Ditch the fatty animal proteins so for lean meats, poultry, and fish. Remember frying is not your friend. If you want to lower the fat content be sure to steam, broil, roast, and bake all your foods.
Hardening of the Arteries and Plaque Build up (Atherosclerosis) Nutrition Interventions
Hypertension and elevated cholesterol can lead to hardening of the arteries and plaque build-up known as atherosclerosis.
Nutrition interventions to improve this condition include a heart-healthy diet that is low
- Sodium
- Saturated fat
- Sugar
An increase in the intake of fiber and antioxidant-rich fruits and vegetables can reduce atherosclerosis.
Electrolyte Imbalances Nutrition Interventions
Nutrition interventions for electrolyte imbalances revolve around regulating minerals that are responsible for maintaining fluid balance. These include
- Sodium
- Potassium
- Phosphorus
When these nutrient levels are regulated electrolyte imbalances will be corrected.
To lower sodium levels you need to limit your sodium intake. Eat foods with little to no sodium by incorporating more fresh whole foods like fruits and vegetables. You can also look for foods with less than 130 mg of sodium per serving.
Reduce potassium levels by avoiding high potassium foods. See the section “Avoid Foods High In Potassium” for more on what foods to ditch.
Limit or avoid foods high in phosphorus to balance electrolyte levels. See the section “Avoid Foods High In Phosphorus” to learn what foods could worsen your CKD.
Toxin Build Up in the Blood Nutrition Interventions
When the kidneys cannot remove wastes from the blood, toxins will build up. This is known as uremia. Good nutrition can help reduce the negative effects of this problem.
Like with electrolyte imbalances, regulating mineral levels of phosphorus, potassium, and sodium can alleviate uremia. Intakes of potassium and sodium should be at 2,000 mg. Phorophsus intake should be at 3,000 mg. However, some individuals may have different needs.
You can reduce your intake of these nutrients by limiting and possibly avoiding foods that contain these nutrients (see the sections below on what foods to avoid).
Be sure to check with your renal RD to know how much potassium, phosphorus, and sodium you should be having.
Nutrients that Improve Uremia
Iron and calcium are two nutrients that can improve uremia. So add some leafy greens and liver to your diet for a boost in these vitamins.
With calcium, you want to make sure you’re eating foods low in phosphorus. This will ensure you pump up the calcium levels.
Since adequate vitamin D status is needed for increasing calcium levels be sure to get enough of this nutrient. You can see the above section “CKD Mineral and Bone Disorder (MBD) Nutrition Interventions” for which foods contain vitamin D.
Depending on your levels you may need to supplement vitamin D, calcium or take a phosphate binder. Be sure to ask your RD if this is necessary before taking anything.
When someone has uremia their protein intake should be restricted unless they are losing protein in the urine.
Recommendations for uremia are under 1 gram for every kilogram of weight. For a person who weighs 100 lb, this would be about 45 grams of protein per day.
For anyone who is losing protein in the urine, they should add one additional gram for every gram of protein that is lost.
Protein intake and waste should be monitored to prevent malnutrition and increase the need for dialysis.
Increased Acid Production Nutrition Interventions
Those with CKD are at risk for increased production of acid. This can lead to a very dangerous condition called metabolic acidosis.
Metabolic acidosis occurs when too much acid is produced by the body. One way to limit acid production is through diet. Incorporating foods that have little to no acid production will lower acid levels and balance the body.
These foods include
- Vegetables
- Fruits
- Beans and legumes
- Some nuts
If you’re curious how to tell if you are at risk for metabolic acidosis check out this post.
Weight Management Nutrition Interventions
One way to prevent CKD from progressing is by managing your weight. Being both over or underweight weight can increase your risk of getting stage 5 of kidney disease.
Good nutrition can help you manage a healthy weight. This means incorporating
- More nutrients into the diet
- Adhering to any restrictions
- Eat more healthy food
- Limit your portions
- Eat less unhealthy fats
- Eat more whole grains
- Have more fruits and vegetables
- Avoid processed and fatty meats
- Add some low-fat dairy but limit phosphorus
- Read food labels to know what is in your food
- Eat less sugar
- Get more fiber
- Drink more water
- Limit alcohol
- Write down what you’re eating daily
- Make a food shopping list and follow it
- Eat before you go shopping
If you’re unsure of how to find a healthy weight, talk to your dietitian and they can help you meet your goal.
Heart Disease Nutrition Interventions
Cardiovascular disease risk can be reduced when other health conditions are managed. So nutrition to reduce for heart disease involves the nutrition interventions as the following conditions:
- High blood pressure
- Anemia resulting from low red blood cell count
- CKD Mineral and Bone Disorder (MBD)
- Diabetes
- Neurological conditions
- Elevated cholesterol
- Hardening of the arteries (atherosclerosis)
- Electrolyte Imbalances
- Toxin build-up in the blood (uremia)
- Increased acid production
- Being over-or underweight
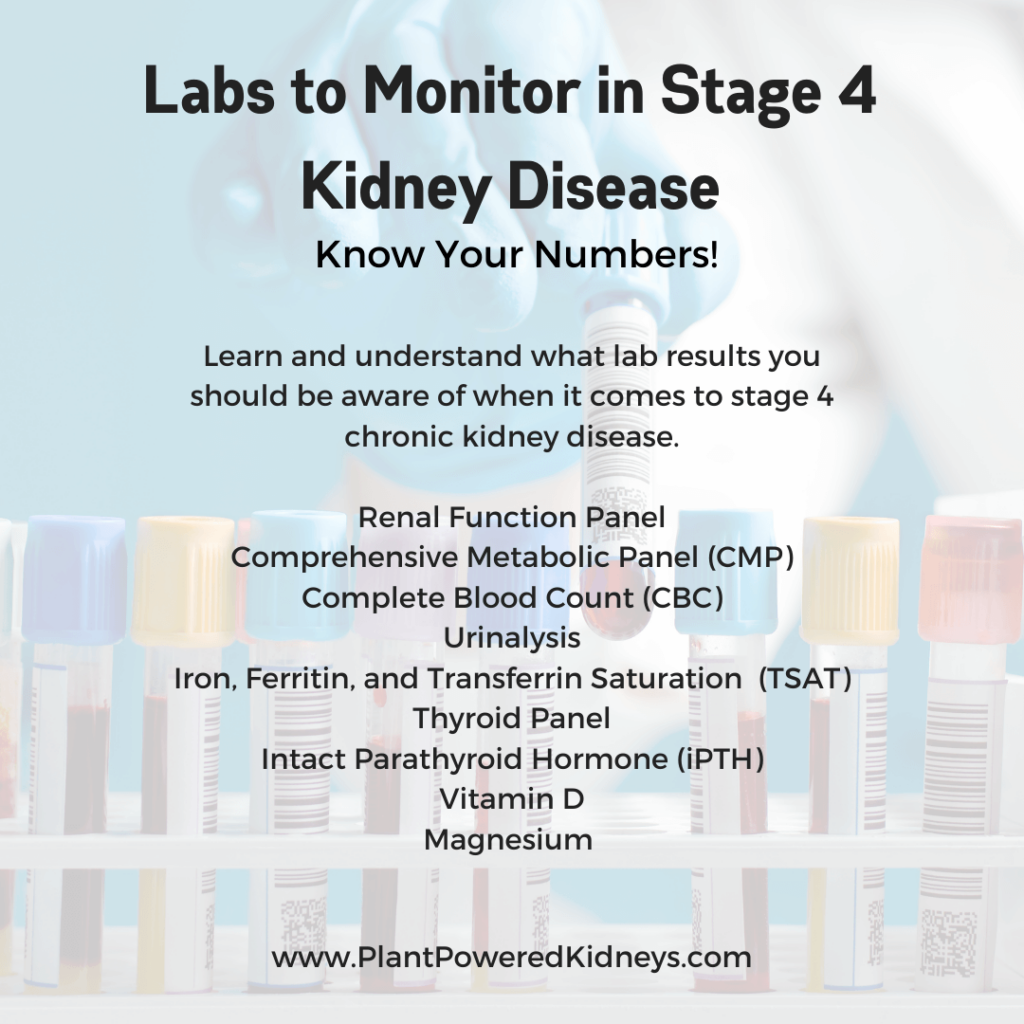
Labs to Monitor in Stage 4 Kidney Disease
Your healthcare team will monitor certain lab values to assess your kidney function and nutrient status. These labs will also help indicate any dietary changes that need to be made to keep your kidney function from worsening. They will keep track of the following:
- Renal Function Panel
- Comprehensive Metabolic Panel (CMP)
- Complete Blood Count (CBC)
- Urinalysis
- Iron, Ferritin, and Transferrin Saturation (TSAT)
- Thyroid Panel
- Intact Parathyroid Hormone (iPTH)
- Vitamin D
- Magnesium
Renal Function Panel
A renal function panel will assess how well the kidneys are functioning during this stage. It looks at the body’s
- Electrolytes
- Minerals
- Proteins
- Glucose (blood sugar)
- Waste products
- Additional calculated values
Electrolytes
Substances in the body with an electrical charge are called electrolytes. We can’t live without them and they are responsible for making nerves and muscles work. They also keep the body’s fluid and acid-base balance. They are made up of
- Sodium
- Potassium
- Chloride
- Bicarbonate (carbon dioxide)
Minerals
Minerals help the body grow and function. Like electrolytes, the mineral phosphorus is needed to prevent metabolic acidosis. Calcium is another essential mineral that is measured. It keeps the heart beating and prevents excessive bleeding.
Protein
Albumin is the protein measured in a renal lab. This substance makes up about 60% of the protein found in the blood. Albumin is needed for heart health. It also transports hormones, vitamins, drugs, and electrolytes, and minerals through the body.
Waste Products
Kidney function is measured by the level of two waste products found in the body. They are
- Urea or blood urea nitrogen (BUN)
- Creatinine.
Blood urea nitrogen (BUN) is a byproduct of protein digestion. Once produced it moves to the kidneys where it is filtered out of the body. The other waste product, creatinine, is made by the muscles. It is also sent to the kidneys for elimination.
High levels of BUN and creatinine can mean poor kidney function.
Glucose (Blood Sugar)
Glucose is also known as blood sugar gives the body energy. The blood will contain a certain amount of glucose on hand that the body can use. When blood sugar is high there is a risk for diabetes.
A urine test can also tell if someone has diabetes.
Blood sugar recommendations vary by person, so ask your renal RD and doctor what are your goals. Typical blood sugar numbers are
- Before meals: 90-130 mg/dL
- Two hours after the start of a meal: below 180 mg/dL
Sometimes your healthcare team will want a larger snapshot of your glucose levels. They will often look at a number called the A1C. This is the 3 month average of your sugar levels. Those with CKD should aim for an A1C of 7%.
Additional Calculated Values
Usually, a renal panel will also contain what is known as the additional calculated values. They are made up of the
- BUN/creatinine ratio
- Estimated glomerular filtration rate (eGFR)
- Anion gap
To get a picture of kidney health your healthcare team will compare BUN to creatinine levels in the blood. A high ratio means the kidneys are not working.
The eGFR is a timed number telling how well the kidneys can filter the blood. It uses creatinine levels and also accounts for the person’s age, race, and gender. Height and weight are possibly included as well.
The anion gap looks at electrolyte levels in the blood. Excess fluid along with low levels of sodium and chloride show kidneys are not functioning well. Dehydration will result in elevations of potassium, sodium, and chloride levels.
Comprehensive Metabolic Panel (CMP)
A comprehensive metabolic panel (CMP) is a test that looks at 14 different compounds in the blood. Most of the test in the CMP is found in the renal panel except for three tests:
- Total Protein
- Liver Enzymes and Bilirubin
- Cholesterol levels
Total Protein
The total protein is the total amount of protein in the blood.
Liver Enzymes and Bilirubin
Liver enzyme function tests measure liver function. They are made up of
- Alkaline phosphatase (ALP)
- Alanine transaminase (ALT)
- Aspartate aminotransferase (AST)
When ALP is elevated it may indicate liver damage.
When AST is high it could suggest
- Heart issues
- Pancreatitis
- Hepatitis (liver inflammation)
- Liver disease
High ALT can also indicate liver damage and disease. These elevations are seen before symptoms start.
This test also measures bilirubin, a compound made by the liver when food is digested. Liver damage may cause bilirubin elevations.
Liver function can be altered by medications, certain foods, supplements, and strenuous exercise. So if you’re bilirubin and liver enzymes are altered it does not necessarily mean there is a problem.
If you’re worried about your liver, ask your doctor what your test results mean.
Cholesterol
Vascular disease is common in CKD so checking cholesterol levels can determine if someone has this problem. This test features the three types of cholesterol. They include:
- LDL the “bad” cholesterol
- HDL the “good” cholesterol
- Triglycerides
This test also looks at total cholesterol which is the sum of the good and bad cholesterol. Ideal cholesterol levels should be
- Total cholesterol should be less than 200
- HDL should be 40 or higher
- LDL should be less than 100
- Triglycerides should be less than 150
If you have elevated cholesterol be sure to discuss a plan to lower your levels with your renal RD and kidney specialist.
Complete Blood Count (CBC) Panel
Individuals with CKD need to check the health of their blood with a complete blood count (CBC). It measures
- Red blood cells
- White blood cells
- Platelets
- Hemoglobin
- Hematocrit
Red Blood Cells Lab Test
Having a low red blood cell (RBC) count causes anemia, iron deficiency, and or heart disease. So checking the RBC levels will help determine what nutrients are needed.
White Blood Cells Lab Test
White blood cells (WBC) are part of the immune system. They are responsible for fighting infections. There are five types of WBC. The WBC portion of the CBC measures the total number of WBC present in your blood.
Sometimes you will get a CBC differential test. This test will measure the total number of each type of WBC in the blood.
If your WBC is abnormally high or low it could mean there is a potential health condition. Alterations in WBC may also be caused by medications, diet, and menstrual cycle in women.
Platelets Lab Test
Platelets are a part of the CBC. These are needed for blood clotting.
The Hemoglobin and Hematocrit Lab Test
The last two lab values in the CBC panel are the hemoglobin and hematocrit. Hemoglobin is a protein in RBC that helps move oxygen from the lungs to body cells. Anemia is caused by low hemoglobin.
Normal levels of hemoglobin in healthy people are
- Women: 12 – 15 g/dL
- Men: 13 – 17 g/dL
People with CKD can have lower hemoglobin levels. Your doctor can tell you what is a good level for you.
The final component of the CBC is the hematocrit. Hematocrit is the amount of blood that is made up of red blood cells. If you have kidney problems your hematocrit will be low.
Urinalysis
Routine urine tests should be done to monitor kidney function and complications like diabetes. This urinalysis looks at the urine’s
- Shade
- Appearance (clear or cloudy)
- Smell
- Its acidity (pH level)
- Presence of bacteria and other germs
A urinalysis will also test for compounds that do not normally belong there including
- Blood
- Protein
- Glucose
- Ketones
- Bilirubin cells
- Crystals
- Tube-shaped proteins called casts
Iron, Ferritin and Transferrin Saturation (TSAT)
Another way to measure iron levels is by looking at the transferrin saturation (TSAT) and ferritin levels tests.
Ferritin is the storage form of iron. The level of ferritin tells how much iron storage is available. Healthy levels are at least 100 ng/mL
The transferrin saturation (TSAT) tells how much of the protein transferrin is in the blood. Transferrin is made by the liver. When the TSAT gets low the liver will make transferrin to overcome the low iron levels.
When TSAT levels fall below 20 percent you could have low iron.
Thyroid Panel
A thyroid panel should be tested every year. Those with thyroid conditions should get tested every three to six months. A full thyroid panel includes the following
- Thyroid Stimulating Hormone (TSH)
- Free Thyroxine (Free T4)
- Free Triiodothyronine (Free T3)
- Thyroid antibodies
- Reverse Triiodothyronine (rT3)
- Signs and Symptoms
- Thyroid Ultrasound
Thyroid-stimulating hormone (TSH) shows how much hormone is made by the thyroid gland.
Free thyroxine (free T4) is the main thyroid hormone. It is tested to see how much free T4 is available for cells to use. It is used with TSH to tell if there is thyroid dysfunction.
Free triiodothyronine (free T3) is another hormone test measuring thyroid function. Like free T4, It is evaluated along with TSH levels.
Reverse Triiodothyronine (rT3) reflects if T4 is being used by the body. It is secreted in small amounts and is a measurement of dysfunction when free T3 is normal but someone still has symptoms.
Medications can also elevate rT3 so check with your medical team to learn about your results.
What the Thyroid Panel Test Results Mean
Results of a thyroid test indicate normal thyroid function when TSH, free T4, and T3 are all normal.
The thyroid can sometimes have abnormalities due to illness. This is known as nonthyroidal illness or sick euthyroid syndrome. It consists of
- Normal OR low TSH
- Normal OR low Free T4
- Free T3 is low
Subclinical hypothyroidism is a mild form of an underactive thyroid. It is also found in people with hypothyroidism on thyroid medications. It is shown by the following:
- High TSH
- Normal FREE T4
- Normal Free T3
Hypothyroidism occurs due to an underactive thyroid and is indicated by the following:
- High TSH
- Free T4 is low
- Free T3 is Normal OR LOW
Hyperthyroidism is when the thyroid is overactive. When there is a problem with the pituitary gland or receptors on the thyroid gland. It is indicated by the following:
- Normal OR high TSH
- High Free T4
- High Free T3
An overactive thyroid that shows no symptoms is called subclinical hyperthyroidism. It can occur from the administration of too much thyroid hormone. It is indicated by the following:
- Decreased TSH
- Normal Free T4
- Normal Free T3
Hyperthyroidism is when the thyroid is overactive. It occurs when there is an
- TSH is low
- Normal OR High T4
- Free T3 is high
Hypothyroidism arising from a problem with the hypothalamus or pituitary gland will show the following:
- TSH is low
- Free T4 is low
- Free T3 is low
Thyroid Panel Test Results Chart
| Thyroid Description | Caused by | TSH Level | Free T4 | Free T3 |
|---|---|---|---|---|
| nonthyroidal illness or sick euthyroid syndrome | illness | Normal OR low | Normal OR low | Low |
| Subclinical hypothyroidism | hypothyroidism on thyroid medications | High | Normal | Normal |
| Hypothyroidism | underactive thyroid | High | Low | Normal OR low |
| Hyperthyroidism | pituitary gland or receptors in the thyroid gland | Normal OR high | High | High |
| subclinical hyperthyroidism | too much thyroid hormone medication | Low | Normal | Normal |
| Hyperthyroidism | overactive thyroid | Low | Normal OR high | High |
| Hypothyroidism | hypothalamus or pituitary gland | Low | Low | Low |
Thyroid Antibody Tests
Antibody tests are used to find the presence of the autoimmune thyroid conditions Hashimoto’s and/or Grave’s disease. They include
- Thyroid peroxidase (TPO) antibodies
- Thyroglobulin antibody (TG) antibodies
- Thyroid-stimulating immunoglobulin (TSI) Antibodies
- Thyroid binding inhibitory immunoglobulin (TBII) Antibodies
Signs and Symptoms to Include in a Thyroid Panel
Aside from blood work, there are physical symptoms that indicate signs of both hypo- and hyperthyroidism.
Signs and symptoms of an underactive thyroid include
- Slowed metabolism
- Weight gain
- Dry skin
- Fatigue
- Constipation
- Fatigue
- Feeling cold all the time
- Muscle weakness
- Weight gain
- Joint or muscle pain
- Anxiety
- Depression
- Brain fog
- Dry skin
- Hair loss
- Slowed heart rate
- Less sweating than usual
- A puffy face
- A hoarse voice
- Women will experience heavy periods
- High LDL cholesterol
Having an overactive thyroid can experience the following signs and symptoms:
- Nervousness
- Tremors of the hands
- Weight loss
- Insomnia
- Puffiness around the eyes
- Irritated eyes
- Bulging eyes
- Increased appetite
- Rapid or irregular heartbeat
- Irritability
- Increased sweating
- Feeling hot
- Muscle weakness
- Diarrhea
- Lighter periods (women only)
- Red, irritated or bulging eyes
- Weakened bones
Thyroid Ultrasound Test
Sometimes a thyroid ultrasound is needed when blood work looks normal and there are no clear signs or symptoms.
Intact Parathyroid Hormone (iPTH)
The intact parathyroid hormone (iPTH) test is used to find the cause of calcium imbalances. It determines
- The cause of high or low calcium levels
- Parathyroid-related calcium imbalances
- Non-parathyroid-related calcium imbalances
- Parathyroid function
- Primary, secondary, and/or tertiary hyperparathyroidism
- Hypoparathyroidism
May also be used to monitor the effectiveness of the treatment when someone has a parathyroid-related condition.
A calcium test always accompanies the iPTH test. It looks at
- The level of calcium in the blood
- The balance between calcium and parathyroid hormone (PTH)
- The response of the parathyroid glands to changing levels of calcium
The reason for the test is to know whether the imbalance is
- Severe and needs medical attention
- Persistent and indicates an underlying problem
What the Calcium and iPTH Test Results Mean
Both the calcium and the iPTH results will be evaluated to determine whether levels are good or if there is something else going on.
A normal iPTH level runs between 10 – 65 pg/mL. The higher the number, the more the kidneys are damaged.
When calcium levels are LOW but PTH levels are HIGH the parathyroid gland is working properly and something else is causing low calcium. Vitamin D, phosphorus, and magnesium may be the cause and can be tested.
LOW calcium with NORMAL or LOW PTH shows parathyroid hormone is not working and there could be hypoparathyroidism. This is when there is dysfunction in the parathyroid gland. It could be due to
- Autoimmune disorder
- Parathyroid damage or removal during surgery
- A genetic condition
- Severe illness
This condition will be accompanied by high phosphorus levels.
If BOTH calcium and PTH levels are HIGH it shows the parathyroid glands are not making enough PTH. This means there is hyperparathyroidism.
There are three glands (primary, secondary, and tertiary) in the parathyroid. There can be dysfunction in different parts of the gland leading to the names primary, secondary, or tertiary hyperparathyroidism.
Imaging and x-rays will determine the cause and severity of this condition.
HIGH calcium with LOW PTH levels means the parathyroid glands are working but there is something else that may be causing elevations in calcium. This could be due to
- Rare mutations in calcium receptors
- Tumors that secrete a PTH-like peptide (will increase calcium and lower PTH)
Vitamin D
Vitamin D testing is ordered when there is kidney disease. This is because poor kidney function is associated with low levels of vitamin D.
The 25-hydroxyvitamin D form is measured to assess and monitor vitamin D status since this is the major form found in the blood and is the precursor to the active hormone 1,25-dihydroxyvitamin D.
It is also ordered to evaluate the effectiveness of calcium, phosphorus, or magnesium supplementation.
Normal levels of vitamin D are above 20 ng/mL. Too much and too little vitamin D can be harmful. Toxicity occurs if levels reach above 100 ng/mL.
Supplementation may be necessary depending on your lab results. Be sure to consult with your medical team for recommendations on supplementation.
Magnesium
Magnesium is a mineral that is needed for energy production, muscle contractions, nerve function, and strong bones. It is found in the diet and stored in bones, cells, and tissues. The test is used to evaluate kidney function.
Abnormal levels are seen in conditions that impair magnesium excretion by the kidneys. So this test will tell how well your kidneys are functioning.
Not having enough magnesium can cause low calcium, potassium. This test is used to diagnose problems with calcium, potassium, phosphorus, and/or the parathyroid hormone.
Too little magnesium can cause
- Changes in heart rate
- Nausea
- Loss of appetite
- Fatigue
- Confusion
- Muscle cramps
- Seizures
- Numbness or tingling
- Worsen calcium deficiencies
Too much magnesium can cause
- Nausea
- Muscle weakness
- Loss of appetite
- Irregular heart rate
The magnesium blood test does not reflect the total body levels. Instead, it is an amount released from bone and tissues. The body does this to keep levels stable.
This means that there could be an early deficiency even with normal blood levels. Certain medications can also increase or decrease magnesium levels.
Drugs that increase magnesium
- Lithium
- Aspirin
- Thyroid medication
- Some antibiotics
These medications will decrease magnesium levels
- Digoxin
- Cyclosporine
- Diuretics
- Insulin
- Some antibiotics
- Laxatives
- Phenytoin
Nutrients to Monitor
To keep the kidneys functioning it is imperative to monitor certain nutrients during stage 4 kidney disease. They include the following:
- Sodium
- Calcium
- Phosphorus
- Potassium
- Magnesium
- Iron
- Fluid
- Protein
Sodium
Sodium is found both in body cells as well as the bloodstream. Our bodies want sodium to be balanced. Fluid moves around until there is a balance of sodium and fluids. So sodium levels are an indicator of your fluid balance.
Normal blood levels of sodium are between 135 and 145 milliequivalents/liter (mEq/L).
When sodium levels are under 135 mEq/L there is too little sodium. This is known as hyponatremia.
When sodium levels are over 145 mEq/L there is too much sodium in the blood. This is called hypernatremia.
Dehydration can cause high levels of sodium. Excessive water intake before the test can alter sodium levels. Edema and fluid retention can also lead to hyponatremia.
If you find your levels are out of range be sure to discuss it with your renal RD to know what if any nutrition changes should be made.
Calcium
The kidneys are responsible for regulating calcium so monitoring this nutrient will tell you how well your kidneys are working. This blood test tells how much calcium is in your blood.
Normal calcium levels range between 8.5 to 10.5 mg/dL (4.3 to 5.3 mEq/L or 2.2 to 2.7 mmol/L). Lab ranges vary up to 0.5 mg/dL
People with kidney disease can experience both hypercalcemia and hypocalcemia. So calcium levels could be both too high and too low.
Calcium should be monitored every 3 months when you have stage 4 kidney disease. If calcium levels are abnormal they need to be evaluated more frequently especially if someone is receiving therapy for issues with calcium, phosphorus, or PTH.
If you have high or low calcium levels, talk to your healthcare team about treatment options before taking any supplements.
Phosphorus
The kidneys control how much phosphorus is in the blood. When they start to decline phosphorus will begin to build up in the blood. So this mineral is measured to determine the health of your kidneys.
Normal phosphorus levels are between 2.5 to 4.5 mg/dL. However, phosphorus ranges can vary from person to person.
Some clinics will use the phosphorus range of 3.0 to 5.0 mg/dL for individuals in the late stages of CKD. Though this can account for the higher phosphorus levels that people with CKD have, the Kidney Disease International Outcomes Guidelines (KDIGO) advise that phosphorus levels should be closer to the normal range to decrease mortality risk.
When you have stage 4 kidney disease phosphorus levels should be checked every 3 months. If your phosphorus, calcium, and/or PTH levels are altered you should get your phosphorus checked more frequently.
If phosphorus levels are above 4.5 mg/dL phosphorus binders may be needed. They should not be taken without medical supervision.
Potassium
Like other nutrients, the kidneys are responsible for regulating potassium levels. When the kidneys are waning in function, they are unable to remove potassium from the blood.
A normal level runs between 3.5 – 5.0 mEq/L. Having too much or too little potassium is dangerous. See the following potassium ranges to know what are the safe and harmful levels
- Safe zone: 3.5 – 5.0 mEq/L
- Caution zone: 5.1- 6.0 mEq/L
- Danger zone: higher than 6.0 mEq/L
Any deviations from the safe zone should be evaluated by your healthcare team so treatment and/or nutrition interventions can be implemented.
Magnesium
The kidneys are needed to regulate magnesium levels. During stage 4 kidney disease, the kidneys’ ability to excrete magnesium declines. So in effect, magnesium can build up in the blood.
Additionally, high magnesium levels can also reduce calcium absorption. This is why magnesium levels need to be monitored.
Normal magnesium levels run between 0.75 and 0.95 millimoles (mmol)/L.
Iron
Iron deficiency is common in those with CKD so iron levels need to be monitored to prevent and improve anemia.
Normal iron levels are between 60 to 170 mcg/dL. Abnormal iron levels can be due to anemia, hepatitis, medications, and for women heavy menstrual periods.
Check with your doctor and healthcare team for reasons why iron levels may be out of range.
As noted above, full iron status is indicated by hemoglobin, ferritin, and transferrin saturation found in the CBC panel.
Fluid
Stage 4 kidney disease typically does not need a fluid restriction but it is still important to monitor fluid levels to know how the kidneys are working.
This is because a lot of fluid in the body indicates poor kidney function.
Fluid restrictions are often prescribed when the kidneys have less than 15% of function, but there could be the need for limiting fluid depending on your health.
A renal dietitian can help you monitor fluid intake to preserve kidney function.
Renal Multivitamin for Kidney Nutrition
Stage 4 kidney disease requires certain nutrients that may not be able to be acquired from diet alone especially when your diet has restrictions that may result in nutrient deficiencies. The nutrients levels needed during CKD are different from healthy individuals so you may need a special renal multivitamin (MV)
A renal MV is a kidney-safe vitamin that does not contain the large toxic doses often found in regular over-the-counter MV. They include the following nutrients:
- Thiamine
- Riboflavin
- Pantothenic acid
- Niacin
- Pyridoxine
- Cyanocobalamin
- Folic acid
- Biotin
- Vitamin C
- Vitamin E
- Iron
- Zinc
- Selenium
- Vitamin D
Most renal multivitamins do not contain large amounts of vitamins A, E, and K. This is done to avoid toxicity from excess vitamin intake. Avoiding these vitamins is recommended unless your doctor prescribes them for you.
Some renal MV recommendations include Renavite and ProRenal +D and omega-3s. This MV gives enough nutrition without the extra nutrients that are hard on the kidneys like vitamin A.
Ask your healthcare team what is the best renal multivitamin for you.
What Foods Should You Avoid with Stage 4 Kidney Disease?
Nutrition plays a major role in preserving kidney function. The diet for stage 4 kidney disease is of utmost importance. It is similar to diets of the other stages with a few more restrictions. This section will answer the question what foods should you avoid with stage 4 kidney disease.
Avoid Sugary Foods and Drinks
Food and drinks with added sugar should be avoided during stage 4 kidney disease. Added sugar is found in processed junk foods, drinks, and even some healthy foods. Juices also contain a lot of sugar and should not be consumed.
Foods with simple sugars have nutritional value. They also increase the risk of type 2 diabetes. These include:
- White breads
- White pasta
- Pastries
- Soda
- Candy
Artificial sweeteners should not be a regular part of the diet. Some research indicates they could increase sugar cravings
Avoid High Sodium Foods
Avoid high sodium foods to preserve kidney function. This will benefit diabetes, kidney disease, and overall health. Reducing sodium can lower blood pressure and prevent fluid retention.
High sodium foods include:
- Table salt
- Soy sauce
- Sea salt
- Teriyaki sauce
- Garlic or onion salt
- Canned foods and soups
- Frozen dinners unless they say “low sodium”
- Ham, bacon, hot dogs, sausage deli, and other processed meats
- Salted snack foods (chips and crackers)
- Dehydrated soups
- Most restaurant foods
- Takeout foods and fast food that is high in salt
- Processed snacks
- Cured meats
- Bacon
- Breads
- Pizza
- Salad dressings
- Pickled vegetables
- Canned vegetables
- Canned beans
- Bouillon
- Salted nuts
- Soups
- Fast food (but there are some that can be okay for CKD!)
Possibly Avoid Foods Fortified with Calcium
During stage 4 kidney disease you may need to avoid foods that are fortified with calcium. These products will increase calcium levels. This is harmful to weakened kidneys because they are not able to clear the excess calcium from the body.
Limit/Avoid High Potassium Foods
When you have stage 4 kidney disease you will need to limit and/or avoid foods high in potassium. The following foods are high in potassium:
- Apricot,
- Acorn Squash
- Bran/Bran products
- Avocado
- Artichoke
- Chocolate
- Banana
- Bamboo Shoots
- Granola
- Cantaloupe
- Baked Beans
- Milk
- Dates
- Butternut Squash
- Molasses
- Dried fruits
- Refried Beans
- Dried figs
- Beets/beet greens
- Grapefruit juice
- Nuts and Seeds
- Kiwi
- Brussels Sprouts
- Peanut Butter
- Mango
- Chinese Cabbage
- Salt Substitutes
- Lite Salt
- Nectarine
- Carrots
- Salt-Free Broth
- Orange(
- Dried Beans and Peas
- Yogurt
- Orange Juice
- Leafy greens (except Kale)
- Snuff/Chewing Tobacco
- Papaya
- Hubbard Squash
- Pomegranate
- Kohlrabi
- Pomegranate Juice
- Lentils
- Prunes/prune juice
- Legumes
- White Mushrooms
- Raisins
- Okra
- Parsnips
- Potatoes
- Pumpkin
- Rutabagas
- Spinach
- Tomatoes/Tomato products
- Vegetable Juices
- Artichokes
- Brussels sprouts
- Sweet potatoes
- Broccoli
- Honeydew
- Black beans
Your renal RD can customize a diet that will give you just enough potassium to keep your kidney health in check.
Limit/Avoid High Phosphorus Foods
Stage 4 kidney disease is an advanced stage of this condition. It is also the point where there is serious damage to the kidneys. As a result, high phosphorus levels will develop.
A way to combat this is to avoid foods that are high in phosphorus. Some food and beverages have phosphorus added to them while others naturally contain phosphorus.
Processed High Phosphorus Foods and Drinks
Most processed foods and drinks that contain phosphorus including the following:
- Ready to eat foods
- Chips
- Crackers
- Pastries and baked goods
- Cereals
- Non-dairy creamers
- Jarred sauces
- Puddings
- Sodas
- Energy drinks
- Juices
- Iced Tea
- Flavored waters
- Lemonades
- Deli meats
- Frozen meats (chicken nuggets, meal kits, etc)
- Seasoned marinated meats
- Processed cheeses
- Products containing aluminum phosphate baking powder
Foods and Drinks Naturally High in Phosphorus
When phosphorus is added to a food or drink, you will be able to see it written on the food label. Turn that product around and see if it contains any of these ingredients:
- Dicalcium phosphate
- Disodium phosphate
- Monosodium phosphate
- Phosphoric acid
- Sodium hexameta-phosphate
- Trisodium phosphate
- Sodium tripolyphosphate
- Tetrasodium pyrophosphate
When in doubt about whether or not a food contains phosphorus check out the food label for the word “PHOS.” If you see it printed there, put it back on the shelf.
Food and beverages with naturally occurring phosphorus that may need to be limited include the following:
If you’re feeling overwhelmed don’t worry. Your renal dietitian can help guide you on what high phosphorus drink and foods to avoid.
Avoid Animal Sources of Protein
A high intake of animal protein can produce a lot of acid and lead to metabolic acidosis. Those with stage 4 kidney disease are at risk for this condition. To prevent acid production these high protein animal products should be limited and/or avoided
- Chicken
- Poultry
- Shellfish
- Beef
- Lamb
- Game meats
- Milk/dairy
- Eggs
Some plant protein sources are very high in protein which could pose a problem for kidney health. The quantity of these foods needs to be limited in a low protein diet. They include
- Tofu
- Tempeh
- Legumes
- Beans
Your renal dietitian can help craft a meal plan that will meet your needs while also giving your kidneys a break from a protein overload.
Avoid Refined Carbohydrates
Carbohydrates are essential in the diet, but avoiding refined carbs can improve kidney health. These carbs are high in sugar. They will negatively affect blood sugar sending it sky-high. Additional pressure on your already poorly functioning kidneys and your stage 4 kidney disease could progress into stage 5.
To prevent blood sugar elevations, limit or avoid these foods:
- Sugar
- White bread
- Pizza dough
- Pasta
- Pastries
- White flour
- White rice
- Sweets
- Desserts
- Breakfast cereals
- Sugary beverages
As always, check with your renal RD to know your carbohydrate needs.
Avoid Unhealthy Fatty Foods
When you have stage 4 kidney disease you need to think about your heart health. The intake of saturated and trans fat are two fats that can increase your risk for high cholesterol and heart disease.
You should avoid foods containing these unhealthy fats. These fats are found in the following:
- Fatty meats
- Pork
- Lamb
- Cheese
- Cow’s milk
- Baked goods
- Butter
- Shortening
- Margarine
- Fried Foods
- Packaged foods
Be sure to read food labels to check for the fat content. The word “hydrogenated” indicates there is trans fat. If you see this word on an ingredient list look for another option that does not contain this fat.
Avoid Alcohol
Alcohol is harmful to those with stage 4 kidney disease because it can lead to
- High blood pressure
- Increased inflammation
- Slow metabolism
- Poor gut health
- Hypoglycemia (a dangerous reduced level of blood sugar)
- Risk of mouth, esophageal, liver, and breast cancer
- Medication interactions
- Altered lab results
- Weight gain
Excess alcohol consumption will put a strain on the kidneys. Some say that one drink a day is ok for those with CKD. One drink consists of the following:
- 12 ounces of beer
- 5 ounces of wine
- 1.5 ounces of liquor
If you have kidney disease and are not already drinking it is advised that you don’t start. Your alcohol recommendations will depend on the individual kidney and overall health. Ask your healthcare team what is right for you. Learn more about alcohol on the renal diet here.
Foods to Eat with Stage 4 Kidney Disease
If you’re feeling like you’re left with nothing to eat. Don’t sweat it! There is still a lot you have even when you’re in stage 4 kidney disease. Read below to find out what you can add to your diet that will help to keep your kidneys rocking.

Foods with Little or No Sodium
Having little to no sodium during stage 4 kidney disease is necessary for health. Decreasing sodium intake can help lower blood pressure and heart disease risk.
There are many low to no sodium option foods. Some foods are naturally low and salt-free while others are made into low and salt-free varieties.
Naturally low and sodium-free foods include the following:
- Dry beans
- Whole grains
- Fresh fruits
- Fresh vegetables
- Frozen fruit with no added dressings or seasoning
- Fresh herbs
- Dried herbs (no salt added)
- Fresh spices
- Dried spices (no salt added)
- Lemon juice
- Low-sodium/salt-free seasoning blends
- Vinegar
- Homemade or low-sodium sauces and salad dressings
- Dry mustard
- Unsalted popcorn
- Unsalted pretzels
- Unsalted tortilla or corn chips
- Low-salt deli meats (unless you have phosphorus restrictions)
- Natural cheese (1-2 oz per week)
- Homemade or low-sodium soups
- Canned food with no added salt
- Homemade casseroles with no added salt
- Fresh meat (beef, veal, pork, poultry)
- Fresh fish
- Fresh eggs
- Rice
- No added sodium pasta
Type of Sodium Food Options
When it comes to foods with added sodium there are a few options you can choose from. They include
- Reduced sodium
- Low sodium
- Very low sodium
- No Salt added
Reduced sodium when a particular food has 25% less sodium than the original product. It still contains some sodium but not as much as its regular counterpart. These types of products still can contain a lot of sodium so read your labels before digging in.
When there is 140 mg or less of sodium per serving in the food is a low sodium food.
Very low sodium means there is just 35 mg or less of sodium per serving.
No added salt means the food product has no added salt. However, there can still be naturally occurring salt that you need to take into account.
Another good tip for looking out for salt on labels. If you see it listed as one of the first few ingredients there is probably a lot of sodium in it. This is because ingredients are listed by weight.
For more low sodium snack ideas check out this post.
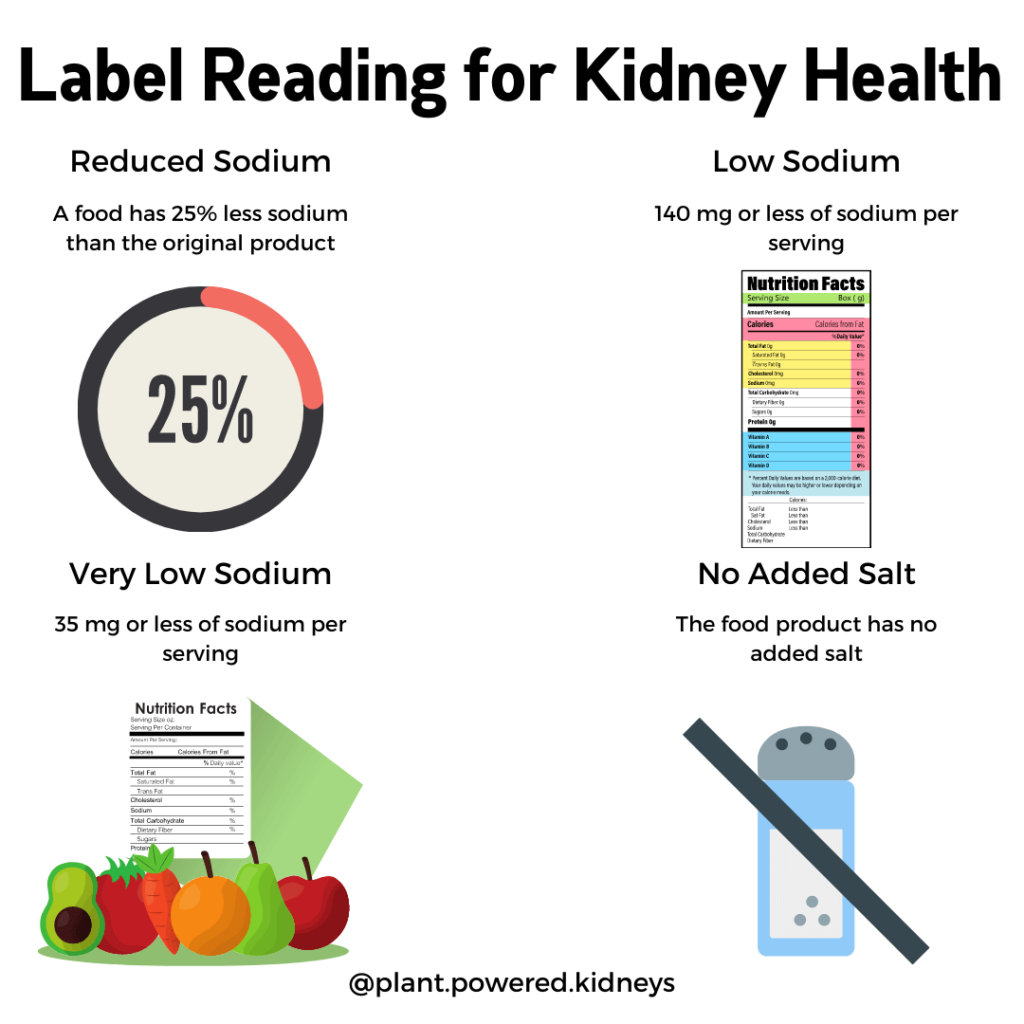
Foods with Less Potassium
Potassium is a dangerous nutrient when too much or too little is consumed. Depending on your labs and own nutritional needs, you may need to strive for a diet of low potassium foods. These include vegetables, fruits, protein, and beverages:
| Low Potassium Vegetables | Low Potassium Fruits | Low Potassium Proteins |
|---|---|---|
| Asparagus Arugula Bamboo Shoots Broccoli Carrots Cauliflower Celery Collard Greens Cucumber Eggplant Green Beans Kale Lettuce Mustard Greens Onion Peas Peppers Radicchio Red Cabbage Scallions Summer Squash (like zucchini) Tomatillo Water Chestnuts White Mushrooms | Apples Applesauce Apricots Blueberries Cherries Cranberries Fruit Cocktail Grapes Lemon Lime Mandarin Orange Pear Pineapple Plum Raspberries Rhubarb Strawberries Tangerine Watermelon | Cottage Cheese Egg Tofu Tuna Pecans Seitan Walnuts |
| Low Potassium Grains | Low Potassium Beverages | |
| Barley Brown Rice Buckwheat Bulgur Plain oatmeal Pasta Popcorn Teff Whole Wheat Bread Wild Rice | Apple juice Coconut Milk Coffee Cranberry juice Ginger ale Grape Juice Lemonade Oat Milk Pineapple juice Rice Milk Tea, brewed |
Things to Consider On Reduced Potassium Diet
If you have protein or fluid restrictions you may need to limit some of these foods and beverages.
Also, don’t overdo it with the serving sizes. You may not realize how much potassium you are getting. A few low potassium foods can add up to big potassium intakes.
If you just can’t live without some of those high potassium vegetables you can try leaching to reduce the potassium content. Ask your renal RD how much-leached potassium you can safely consume during this stage of CKD.
As always, this is a blanket recommendation. Ask your dietitian about your specific potassium needs before changing your diet.
Learn more about low potassium diets here.
Reduced Phosphorus Foods
People with stage 4 kidney disease may need to have a phosphorus restriction. So the diet should be limited to only low phosphorus foods to maintain kidney function.
Foods that have less phosphorus include the following:
- Fresh fruits and vegetables (see all of these in this post)
- Whole grains (see all the low phosphorus whole grains here)
- Plant Proteins (tofu, soybeans, tempeh edamame, nuts, seeds, beans, legumes,)
- Egg whites (depending on protein needs)
- Beverages (black coffee, brewed tea, fruit juices ginger ale, some milks/soda/teas)
Like with potassium, eating too many low phosphorus foods could still elevate blood levels of phosphorus.
So stick with serving sizes especially when it comes to nuts, seeds, and nut butters. These foods tend to get overeaten without even realizing it. Eat just ¼ cup for nuts and seeds. Nut butter servings consist of 2 tbsp.
If you’re concerned about your phosphorus levels, ask your renal RD about a phosphorus plan that will help your kidneys thrive. You may also need phosphorus binders to help control your phosphorus levels.
Calcium-Rich Foods (with No Potassium and/or Phosphorus)
People with stage 4 kidney disease need calcium especially if they have issues with bone health or vitamin D absorption.
A lot of calcium-rich foods are also high in potassium and phosphorus. This becomes problematic for people who have nutrient restrictions.
One way to avoid overdoing it on potassium and phosphorus is by adding foods like kale, arugula, tofu, and sardines to the diet. These foods should elevate calcium levels without altering other nutrients.
Reduced Protein and Plant Protein Foods
Studies have found that eating less protein may improve stage 4 kidney disease. This diet has shown to have the following benefits:
- Prolong kidney function
- Decrease acid production and risk of metabolic acidosis
- Reduce protein levels in urine
- Alleviate oxidative stress
- Reduce blood pressure
- Improve insulin resistance
- Minimize uremia toxins
- Regulate phosphorus levels
A low protein diet can be one where the protein is spread out and combined with other foods to make for a satisfying meal. This keeps protein as a side dish and accentuates foods that will fill you up like vegetables and whole grains.
Some examples of this are adding
- Vegetables to a sandwich with less meat
- Add milk substitutes to cream soups, rice, and pasta
- Make meat your side only, bulk up the meal with vegetables
- Mix plant protein grains with vegetables and just a touch of meat
- Make your casserole almost meatless
- Take your meat soups and make them starchy
- Use a bit of strong cheese to flavor your dishes
Alternatively, this type of diet will be heart-healthy highly plant-based (potentially low-potassium options). This will be a large variety of grains, fruits, vegetables, and healthy fats (learn more about healthy fats below).
Becoming a vegetarian or vegan will also decrease your protein intake. Learn more about reducing protein in your diet here.
Complex Carbs and Foods High In Fiber
Complex carbs and foods high in fiber are great for controlling stage 4 kidney disease. They regulate blood sugar, blood pressure, and take longer to digest. This means you will be fuller longer.
Complex carbohydrates and fiber are found in vegetables, fruits, and whole grains.
It is recommended to get at least 6 servings of whole grains per day. These include:
- Whole grain pasta
- Brown rice
- Barley
- Quinoa
- Millet
- Couscous
- Brown rice
- Wild rice
- Oats
- Quinoa
- Farro
- Freekeh
- Sorghum
- Tapioca
- Millet
- Barley
- Durum
- Buckwheat
- Teff
- Arrowroot
- Wheat berries
- Kamut
- Amaranth
- Bulgur
- Whole wheat bread, bagels, and buns
If you have questions about your carbohydrate intake ask your renal dietitian for recommendations based on your kidney health.
Healthy Fat Foods
The body cannot survive with adequate fat intake. However, the type of fat you eat can make or break your kidney function. That is why healthy fats need to be part of the stage 4 kidney disease nutrition intervention. They include
- Monounsaturated (MUFAs)
- Polyunsaturated (PUFAs)
MUFA and PUFAs help lower cholesterol and heart disease risk. MUFAs also lower the bad “LDL” cholesterol. PUFAs consist of the essential fats omega-6 and omega 3. The body cannot make them and they must be acquired from the diet. Some of the foods with these healthy fats include
- Olive oil
- Avocado oil
- Sesame oil
- Chia seeds
- Ground flaxseeds or flaxseed oil
- Walnuts
- Pecans
- Macadamia nuts
- Avocado
- Hemp hearts
- Olives low in sodium
- Peanut butter
- Salmon
- Mackerel
- Herring
- Trout
Saturated fats should be replaced with these heart-healthy fats to preserve kidney function as well as lower the risk of heart disease.
If you’re looking for specific fat recommendations based on your health status have a chat with your renal RD about where to get the best sources of healthy fat.
Stage 4 Renal Diet Meal Plan
If all these restrictions are a bit overwhelming check out our sample stage 4 kidney disease renal diet meal plan to learn what possible foods you can add to improve the health of your kidneys.
Please know this is only a sample. There is no one right eating plan for everyone. Depending on your kidney health, underlying conditions, and the levels of nutrients like protein, sodium, potassium, phosphorus, and calcium will determine what type of diet will help you best.
If you want a more comprehensive stage 4 kidney disease diet plan you should meet with a renal RD. They can create an individualized meal plan tailored specifically to meet your nutritional goals.
Life Expectancy with Stage 4 Kidney Disease
Many people ask how long can you live with kidney disease? This varies by the stage of the disease and how well someone is managing any underlying conditions.
As discussed above, stage 4 kidney function ranges from between 15 and 29 percent. For men and women with less than 30 percent kidney function, life expectancy was substantially reduced when compared with earlier stages of kidney disease.
Age and Gender Effects Life Expectancy in Stage 4 Kidney Disease
When it comes specifically to what is the life expectancy of someone with stage 4 kidney disease, age and gender seem to be determining factors.
According to research, age and, to a slighter degree, gender both play a role in stage 4 kidney disease life expectancy.
With stage 4 kidney disease, the older you are the shorter your lifespan becomes. The following are life expectancies for a 30, 40, 50, 60, 70, and 80-year-old man and women:
| Age at Diagnosis | Estimated Life Expectancy for Males (years) | Estimated Life Expectancy for Females (years) |
|---|---|---|
| 30 Yrs Old | 15.3 | 12.7 |
| 40 Yrs Old | 10.4 | 9.1 |
| 50 Yrs Old | 7.4 | 7.4 |
| 60 Yrs Old | 5.6 | 6.2 |
| 70 Yrs Old | 3.9 | 4.1 |
| 80 Yrs Old | 2.5 | 3.1 |
In other stages of CKD, women were seen to live longer. However, when it came to life expectancy, stage 4 kidney disease there was only a slight difference between the genders. Men had a longer lifespan until the age of 50. Then women slightly outlived men.
Please know this is only an average and the specific prognosis for CKD depends on how well the disease and its associated complications are being managed. If you’re concerned about your mortality risk, ask your healthcare team what can be done to prolong your life.
Summary
Stage 4 kidney disease is the point when kidney function has surpassed the middle ground. Although there is severe kidney damage that cannot be repaired, there is still a lot you can do to resuscitate your kidney health. This starts by assessing your CKD along with its associated health conditions and/or complications that may be present.
Incorporating medical, nutritional, and lifestyle interventions will improve CKD and its associated conditions. It can also decrease the potential for future problems like dialysis and/or a kidney transplant.
Take charge of your health by getting a team of healthcare professionals who can monitor labs, nutrient levels, and offer a customized nutrition and medical plan that will help you thrive.
As a reward for all your hard work, you will notice an improvement in blood pressure, diabetes, anemia, heart disease, and other underlying health conditions.
Related Posts
Here are some other articles related to stage 4 ckd that may be of interest to you!


Hi Jen
I have been diagnosed CKD Stage 4. I would like your assistance in tailoring a diet and meal plan. My blood sugar and hypertension is under control. If necessary, I can make my blood work available for your review. Please contact me to further discuss treatment options.
Regards,
Cazim.
Hi Cazim! You can reach out to our team of dietitians to learn more about working with us one-on-one.
Article on CKD 4 is very much informative.
We’re so happy to hear that! Thank you, Mahender! 🙂
I won’t meet with a nephrologist until May 30, 2023.The last set of lab tests finds me anemic with a EGFR of 24. What suggestions do you have for me.
I just found out this set of lab tests and as of today I have started with suplementing using cereal my iron, vitamin B12, and folate. I will read the articl on ckd 4.
Hi Juan! The best advice we can give is to work with a dietitian for quick, personalized guidance. A dietitian can tell you how much protein, potassium, sodium, and even phosphorus you need to protect your kidney health. Some in stage 4 also find our PPK Course to be helpful as we cover these topics. You can sign up for the waitlist here to get an email invitation to join.
Dear Jen, Please I need your help! My husband is in CKD Stage 4 and I’m asking from far away from your country. We are at the Kingdom of Tonga, and I am looking for a food its good for my husband for his kidney disease. Can you please tell me what food for his breakfast, lunch and dinner. We will count a blessing in your help. May God Bless you, and y our family.
Hi Vika, thank you for reaching out. It’s so touching to hear how much you care about your husband’s health. We cannot provide personalized plans in this setting, unfortunately. We do offer sample meal plans that you may find useful. Click here to take a look. 💚