When you think of the words “minerals and kidney disease” or “electrolytes and kidney disease” what do you think of?
Do you just think of sodium, potassium and phosphorus, or do you think about things like calcium, magnesium or selenium?
Sodium, potassium and phosphorus are the three main mineral and electrolyte players when it comes to influencing kidney health.
Additionally, we are going to cover much more than just that in this article. We’ll include magnesium and kidney disease, calcium and kidneys, electrolytes and kidney function and more!
If you missed the first two parts of this multi-series guide, you can get all the information you need to know about B vitamins for kidneys here and vitamin D and the fat-soluble vitamins here.
This article contains affiliate links in which I earn a small percentage of sales. As an Amazon Associate I earn from qualifying purchases, at no expense to you. This supports my website and ability to write up more helpful content – thank you for your support!
Please note: the dosage recommendations in this post are based off of the Dietary Reference Intakes (DRIs), which include Adequate Intake (AI), Recommended Daily Allowance (RDA), and Estimated Average Requirements (EAR) that are developed by the Institute of Medicine and serve as a base guideline for vitamins and minerals in this article. Recommendations are not meant to be taken as medical advice. Talk with your medical provider about what dosages are right for you.
Table of Contents
What are minerals?
Minerals (and vitamins) are essential organic substances needed in small amounts in a diet. However, unlike protein, fats, and carbohydrates, minerals are not a source of energy. In other words, they do not contain calories.
Rather, they aid in energy metabolism. This means they help you get the energy you want out of your food by playing a part in the chemical reactions that take place in your body when digesting food.
They are also part of what keeps you hydrated in the form of electrolytes. We give them this name because they actually have an electric charge! The main thing they “power” is water moving in and out of cells to maintain a proper fluid balance. They also aid in muscle contraction.
Humans cannot produce minerals, unlike certain vitamins, and we must rely on consuming them through our diet.
How do I know if I need to take any minerals or electrolytes for kidney disease?
Those with chronic kidney disease (CKD) may need higher or lower amounts of certain vitamins and minerals, especially for patients who are on dialysis. Your nephrologist or RD should let you know if you should be taking supplements. Your doctor can order a micronutrient lab panel to test your values.
Additionally, you can take a micronutrient deficiency test, such as Spectracell, which tests for 31 vitamins, minerals, amino and fatty acids, antioxidants, and metabolites. This test may require a physician order.
More importantly, you can then bring your results to your medical provider and they can give you more guidance on which supplements would be best for you.
Minerals and Chronic Kidney Disease
There is no single “best” vitamin or mineral for patients with CKD. However, there are some that are more commonly deficient than others. People with CKD often have a higher need of water-soluble vitamins & certain minerals. Those with CKD should be wary of taking excess amounts of fat-soluble vitamins, as overconsumption can cause toxicity in the body.
Minerals
Magnesium
Function
Magnesium is required for energy production, creating DNA, muscle contraction, normal heart rhythm and nerve communication.
It is also reputably known for its calming effects and is often marketed this way in supplement form. Studies suggest that magnesium supplementation may be effective in reducing stress and anxiety, however, it is claimed that the quality of evidence is poor.
Sources
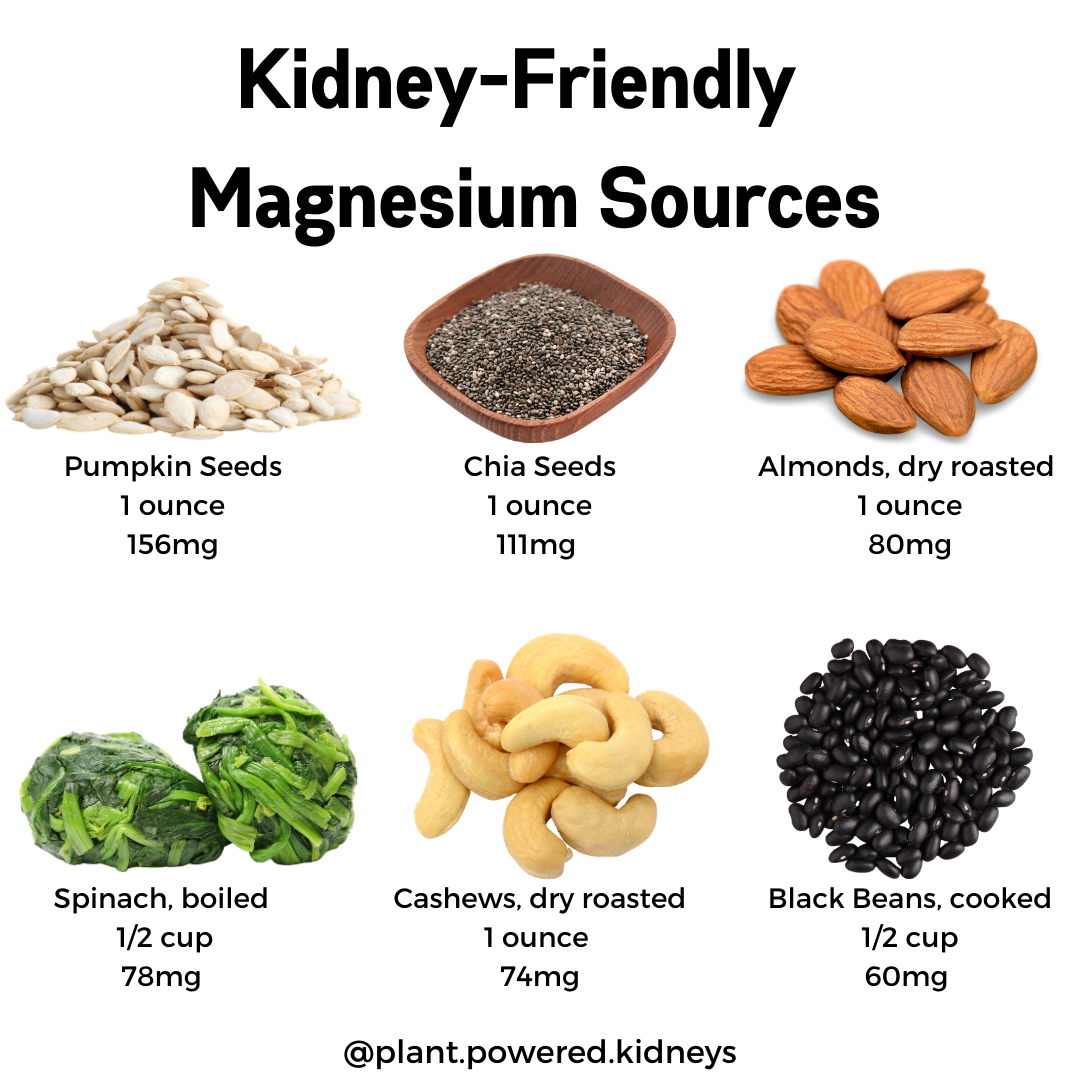
Magnesium can be found in both plant and animal foods, however the concentration in plant foods is much higher. Certain nuts & seeds and dark, green leafy vegetables are among the best sources of magnesium.
See the table below for a list of food sources of magnesium.
Table 1. Food sources of magnesium
| Food | Milligrams (mg) per serving |
| Pumpkin seeds, roasted, 1 ounce | 156 |
| Chia seeds, 1 ounce | 111 |
| Almonds, dry roasted, 1 ounce | 80 |
| Spinach, boiled, ½ cup | 78 |
| Cashews, dry roasted, 1 ounce | 74 |
| Black beans, cooked, ½ cup | 60 |
| Rice, brown, cooked, ½ cup | 42 |
Forms of Magnesium
You can find magnesium supplements in various forms, including magnesium oxide, citrate and chloride. All of these forms absorb differently in the body, some better than others.
Some studies have shown that the aspartate, citrate, lactate, and chloride forms absorb better than magnesium oxide or sulfate. Of course, if you can’t remember all these names, just note that forms of magnesium that dissolve in liquid are absorbed better.
Drug-Nutrient Interactions with Magnesium
There are several types of medications that can affect magnesium levels in the body, including, some diuretics.
- Bisphosphonates (used to treat osteoporosis)
- Antibiotics (DeclomycinⓇ, VibramycinⓇ, CiproⓇ, LevaquinⓇ)
- Diuretics
- Proton Pump Inhibitors (NexiumⓇ, PrevacidⓇ)
Recommended Intake and Deficiency
The recommended daily intake of magnesium for males 14-18 years is 410mg, then decreases to 400mg for those 19-30 years, and is 420mg for 31 years and older.
For women 14-18 years, 360mg a day is recommended and decreases to 310mg for those 19-30 years. For ages 31 and up, 320mg a day is recommended.
Many people in the US consume less than the recommended daily amount of magnesium. Signs and symptoms of a mild deficiency include nausea, vomiting, fatigue, and weakness. As the deficiency gets more severe, one may experience muscle contractions and cramps, seizures, abnormal heart rhythms, numbness, and tingling.
Tolerable Upper Level Intake
For the average, healthy person high magnesium intake is not of much concern since the kidneys excrete any excess magnesium in the body. However, with magnesium and kidney disease this ability is diminished.
High doses of magnesium from supplementation can be accompanied by diarrhea, nausea, and abdominal cramping. Severe magnesium toxicity can include signs such as facial flushing, retention of urine, irregular heartbeat and cardiac arrest.
What is so important about Magnesium and Kidney Disease?
Depending on what level of function your kidneys have, you may find yourself with either higher or lower levels of magnesium. Low levels of magnesium are associated with a higher risk of progressing towards end-stage kidney disease, while high levels are linked with those who already have more advanced CKD.
One study has suggested that magnesium supplementation may counteract the negative effects of phosphate overload in kidney disease, however it has not been clinically tested yet.
Supplementation may also be protective against heart disease in those with CKD, yet larger trials are required.
Taking certain types of diuretics can increase the amount of magnesium your body excretes through urine, while other potassium-sparing diuretics reduce this chance. If you aren’t sure which kind you are taking, speak to your medical provider.
Before you reach for a bottle of magnesium supplements just because it says it will “calm” you, check with your doctor about if taking them is right for you. Those in the later stages of CKD have a harder time filtering out excess minerals in the body and you may be more susceptible to a build-up of magnesium in this case.
Iron
Function
Iron is an essential component in the making of red blood cells. It is also required for growth, neurological development, and the synthesis of some hormones.
Sources
There are two different types of iron, heme and non-heme. Heme sources of iron come from animal-based products like meat and seafood. Non-heme sources come from plant-based products like legumes, vegetables, and fortified grain products such as breakfast cereals.
The list below includes sources for both heme and non-heme iron.
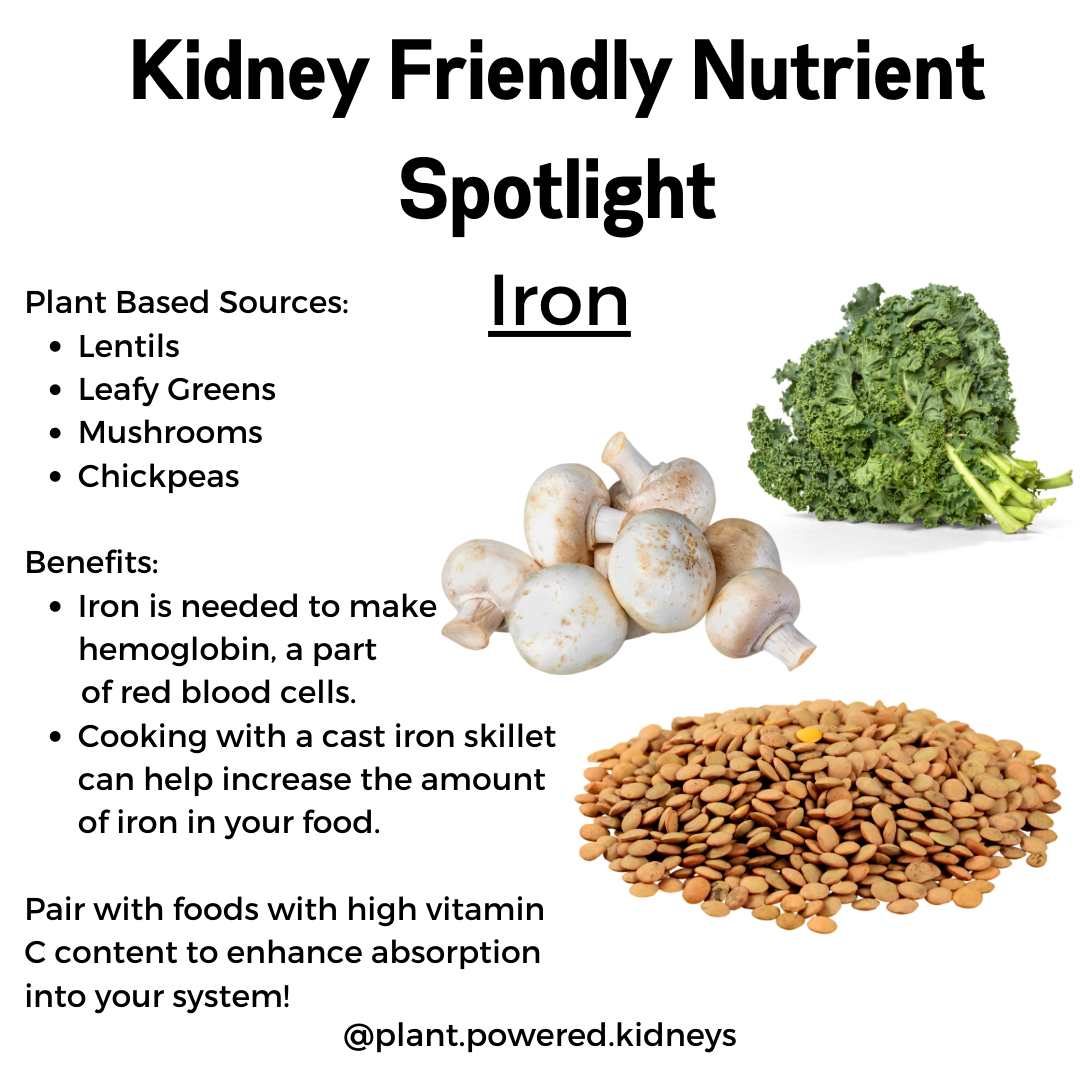
Table 2. Food sources of iron
| Food | Milligrams (mg) per serving |
| Breakfast cereals, fortified with 100% Daily Value for iron, 1 serving | 18 |
| White beans, canned, 1 cup | 8 |
| Chocolate, dark, 45-69% cacao solids, 3 ounces | 7 |
| Lentils, boiled and drained, ½ cup | 3 |
| Spinach, boiled and drained, ½ cup | 3 |
| Tofu, firm, ½ cup | 3 |
| Chickpeas, boiled and drained, ½ cup | 2 |
| Tuna, light, canned in water, 3 ounces | 1 |
| Chicken, roasted, meat and skin, 3 ounces | 1 |
Forms of Iron
As mentioned prior, there are two different forms of iron. Heme iron sources come from meat, seafood and poultry. Non-heme iron sources come from vegetables and fortified food products like breakfast cereals.
The body absorbs heme iron much better compared to non-heme iron. Some non-heme sources contain other naturally-occurring chemicals that inhibit the absorption of iron, making it harder for your body to get the full iron content out of the food.
For example, spinach contains certain polyphenols, which are packed with antioxidants and provide a wide range of health benefits. Unfortunately, they are also an inhibitor for iron absorption. It is also suspected that calcium interferes with iron absorption, so you may want to consider not eating calcium and iron rich foods together in the same sitting.
In supplements, you will commonly find ferrous and ferric iron salts as the source of iron. Comparatively, ferrous is absorbed better in the body, so this could be something to be on the look out for if you are purchasing a supplement.
Drug-Nutrient Interactions with Iron
Iron can react with some medications, and some medications may affect iron levels in the body.
- Levodopa (SinemetⓇ, StalevoⓇ)
- Levothyroxine (treatment for hypothyroidism)
- Proton pump inhibitors (PrevacidⓇ, PrilosecⓇ)
Recommended Intake and Deficiency
The recommended daily intake of iron for men is 11mg for 14-18 years old and 8mg for 19-50+ years. For women, it’s 15mg for 14-18 years old, 18mg for 19-50 years, and 8mg for 51+ years.
Majority of people get an adequate amount of iron each day. However, it’s not unusual for someone to be iron deficient in the US, especially in women of childbearing age, children, and pregnant women. Those with CKD are also at increased risk of deficiency.
A mild deficiency would be diagnosed by decreased iron concentration in the blood and bone marrow. Moderate deficiency results in depleted iron stores, while hemoglobin levels remain in normal ranges. Severe deficiency, also known as iron deficiency anemia, is presented with declined hematocrit and hemoglobin levels, and is usually characterized by small red blood cells.
Tolerable Upper Level Intake
Consuming too much iron can result in uncomfortable to deathly consequences. Intake of more than 20mg per kilogram of body weight can cause gastric upset, nausea, vomiting, and faintness. Drastic intakes of 60mg per kilogram of body weight have been known to cause organ failure and even death.
The official upper level intake for iron set by the Food and Nutrition Board (FNB) is 45mg/day for both men and women 14 years and older.
Why is iron important for kidney disease?
Iron deficiency anemia is very common in CKD patients, and the risk increases as kidney functionality decreases. You need sufficient iron so our bodies can produce enough red blood cells to deliver oxygen to tissues and carry out carbon dioxide.
Patients who are on hemodialysis have a greater iron loss and are frequently treated with erythropoiesis-stimulating agents. These are agents that work to help create hemoglobin, which is the oxygen carrying molecule on red blood cells.
You can work to prevent iron deficiency anemia in the first place by incorporating iron-rich foods in your diet, pairing them with vitamin C-rich foods, and cooking with cast iron cookware. Click here to read more about anemia and CKD.
Copper
Function
Copper helps your body absorb iron and is also required to form red blood cells. It is also involved in brain development, immune system support, and creating connective tissue, such as collagen.
Sources
Copper can be found in both animal and plant-based foods. The highest food sources of copper include shellfish, seeds, nuts, cacao, and fortified foods.
See Table 3 for a list of food sources of copper.
Table 3. Food sources of copper
| Food | Micrograms (mcg) per serving |
| Oysters, eastern, wild, cooked, 3 ounces | 4,850 |
| Mushroom, shiitake, cooked, cut pieces, ½ cup | 650 |
| Cashews, dry roasted, 1 ounce | 629 |
| Crab, dungeness, cooked, 3 ounces | 624 |
| Dark chocolate, 70-85% cacao solids, 1 ounce | 501 |
| Tofu, raw, firm, ½ cup | 476 |
| Millet, cooked, 1 cup | 280 |
| Avocado, raw, ½ cup | 219 |
Forms of Copper
If you are shopping for supplements, you may find copper in the form of cupric oxide, cupric sulfate, copper amino chelates, and copper gluconate. Unfortunately, there are no known studies that compare the absorption rates of these forms.
Drug-Nutrient Interactions with Copper
As of now, there is little known about the interactions copper has with medications. Regardless, it is always important to consult your doctor before starting a new supplement routine.
Recommended Intake and Deficiency
The daily recommended intake for copper for both men and women is 890mcg for those 14-18 years old and increases to 900mcg for those 19 years and older.
Copper deficiency is rare in humans. A deficiency in copper can present itself with anemia, hypopigmentation, high cholesterol, connective tissue disorders, osteoporosis, and increased risk of infection.
Tolerable Upper Level Intake
Copper toxicity is rare in otherwise healthy individuals. However, long-term exposure to high levels of copper, such as high levels in drinking water, can lead to liver damage and gastrointestinal symptoms.
The FNB has established the tolerable upper level intakes for copper at 8,000mcg for men and women 14-18 years old and 10,000mcg for men and women 19 years and older.
Why is copper important for kidney disease?
Luckily, multiple studies suggest that copper levels are mostly unaffected by CKD. At the same time, this doesn’t mean that you should just ignore your copper intake all together.
As mentioned earlier, copper is an essential mineral in carrying out the processes in conjunction with iron to create red blood cells. Consequently, consuming an adequate amount of copper in your diet can help to prevent iron deficiency anemia.
Selenium
Function
Selenium is essential for proper thyroid hormone metabolism, DNA synthesis, and contains many antioxidant properties.
Sources
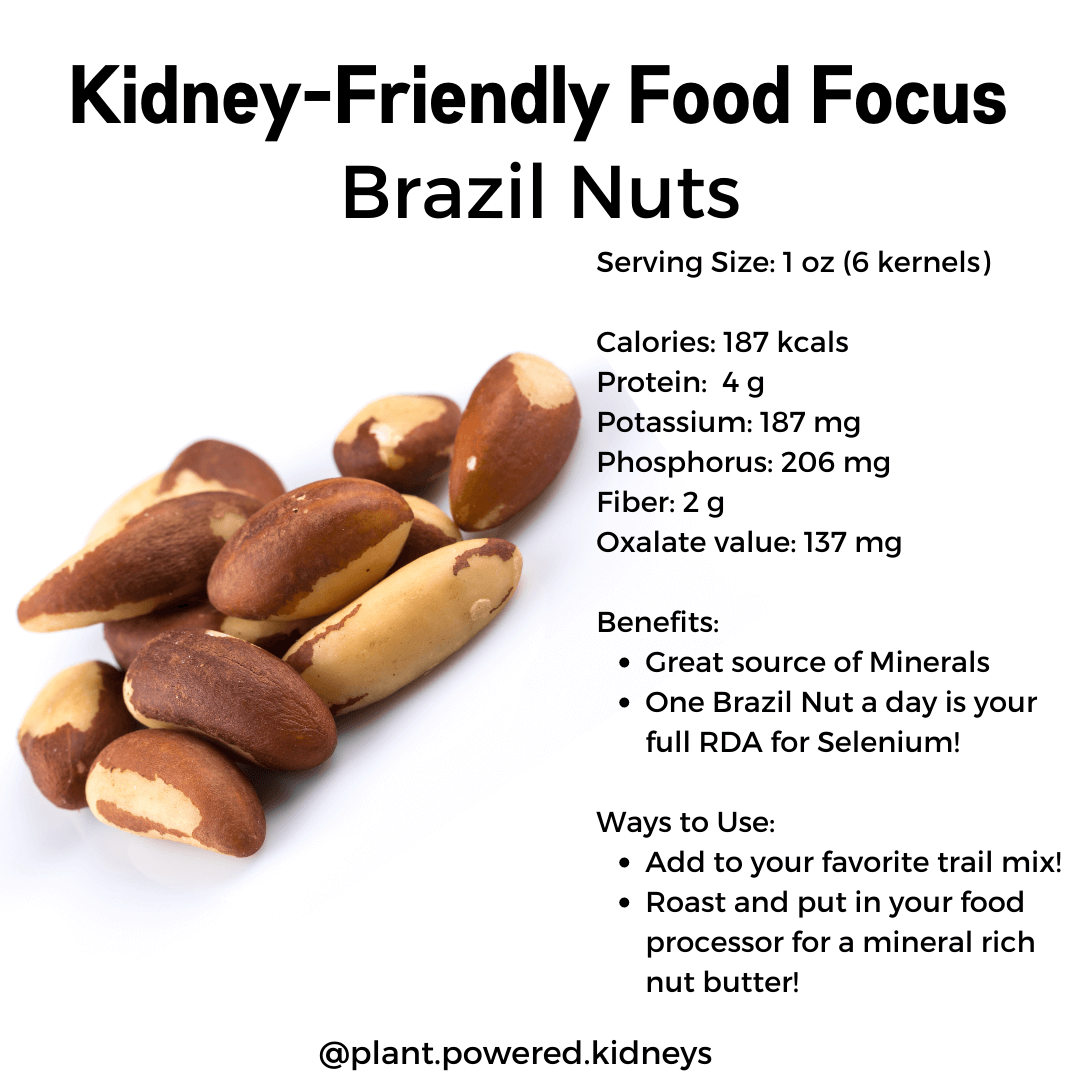
Some of the best food sources of selenium includes brazil nuts, seafood, and organ meats.
See Table 4 for a list of great sources of selenium.
Table 4. Food sources of selenium
| Food | Micrograms (mcg) per serving |
| Brazil nuts, 1 ounce (6-8 nuts) | 544 |
| Halibut, cooked, dry heat, 3 ounces | 47 |
| Ham, roasted, 3 ounces | 42 |
| Macaroni, enriched, cooked, 1 cup | 37 |
| Rice, brown, long-grain, cooked, 1 cup | 19 |
| Baked beans, canned, 1 cup | 13 |
Forms of Selenium
Selenium can either be organic (selenate and selenite) or inorganic (selenomethionine and selenocysteine). Both of these forms are good sources of selenium. Typically the soil in which plants grow contains the inorganic form and as the plants grow and take in the nutrients from the soil, they convert it into the organic form.
Most selenium in the body is in inorganic form, stored mainly in the muscle.
In supplements, selenium is usually sold in the selenomethionine form as the human body is able to over 90% of it in this way.
Drug-Nutrient Interactions with Selenium
Some medications may adversely affect selenium levels in the body, and selenium may interact with certain medications. Be sure to consult your doctor before starting or changing your supplement routine. An example of a medication that is known to be affected by selenium is listed below.
- Cisplatin (for treatment of various cancers)
Recommended Intake and Deficiency
The daily recommended intake of selenium for both men and women 14 years and older is 55mcg.
Most people in the US consume an adequate amount of selenium. A deficiency in selenium has been associated with depressed mood, anxiety, predisposal to developing other illnesses, and male infertility.
Tolerable Upper Level Intake
Excessive consumption of selenium can at first result with a garlic breath odor and a metallic taste in the mouth. The most characteristic sign of high intake is hair and nail loss and brittleness.
Severe selenium toxicity can result in gastrointestinal and neurological symptoms, acute respiratory distress syndrome, and kidney failure. The set tolerable upper level intake for selenium for both men and women 14 years and older is 400mcg.
Why is selenium important for kidney disease?
Low selenium levels are common in CKD patients, especially in those who are on hemodialysis.
The research on the effects of selenium supplementation and kidney disease is limited but promising. Studies suggest that low selenium levels may contribute to immune dysfunction, therefore putting hemodialysis patients at higher risk of infectious diseases. Fortunately, oral and intravenous supplementation of selenium showed significant reductions in oxidative stress.
Phosphorus
Function
Phosphorus is a main component of bones, teeth, DNA and RNA. It is also required to build the cell membrane structure and is part of the body’s main energy source.
Sources
Animal based foods, specifically dairy, is the biggest contributor to the average person’s phosphorus consumption. They are especially prevalent in processed foods as phosphate additives are commonly used as a preservative.
See Table 5 for a list of food sources of phosphorus.
Table 5. Food sources of phosphorus
| Food | Milligrams (mg) per serving |
| Yogurt, plain, low-fat, 6 ounce container | 245 |
| Milk, 2% milkfat, 1 cup | 226 |
| Salmon, Atlantic, farmed, cooked, 3 ounces | 214 |
| Cheese, mozzarella, part skim, 1.5 ounces | 201 |
| Chicken, breast meat, roasted, 3 ounces | 182 |
| Lentils, boiled, ½ cup | 178 |
| Potatoes, russet, flesh and skin, baked, 1 medium | 123 |
Forms of Phosphorus
When in supplements, phosphorus is usually found in the form of phosphate salts such as dipotassium phosphate or disodium phosphate. The body absorbs about 70% of the phosphorus in this form.
Drug-Nutrient Interactions with Phosphorus
Phosphorus can interact with certain medications, and some medications can affect phosphorus levels in the body. Examples are listed below.
- Antacids (containing aluminum hydroxide)
- Laxatives (containing sodium phosphate)
Recommended Intake and Deficiency
The recommended daily intake for the otherwise healthy person is 1,250mg for ages 14-18 and 700mg for ages 19 and up.
However, if you are living with decreased kidney function, these are not the daily goals you should be aiming for. It is important to talk to your doctor or renal dietitian about what your phosphorus intake goals should be.
Phosphorus deficiency is rare in the US, likely because so many processed foods use phosphates as a preservative. Cases of deficiency are often caused by a disease state such as diabetic ketoacidosis or kidney tubule defects rather than inadequate intake.
Signs and symptoms of deficiency include anorexia, muscle weakness, impaired coordination, osteomalacia, and increased infection risk.
Tolerable Upper Level Intake
High consumption of phosphorus in the average healthy person rarely causes adverse health effects. Although, there have been links between intakes of 1,000mg/day or higher and adverse cardiovascular, kidney, and bone effects.
The tolerable upper level intake for phosphorus is 4,000mg for those ages 19-70 years and 3,000mg for those 71 years and up.
Why is phosphorus important for kidney disease?
Those with kidney disease probably know that one of the first things to start staying away from in the diet is phosphorus. This is because normal functioning kidneys are able to rid of excess phosphorus, while damaged and diseased kidneys cannot, easily causing a build-up of phosphorus in the body.
The relationship between phosphorus and kidney disease is deep-rooted and can be confusing to learn about, especially in regards to what to eat to keep your lab levels in a healthy range. You can read all about the details in this two-part guide to phosphorus and your diet by clicking here for part one and here for part two.
Calcium
Function
Calcium is the most abundant mineral in the body. It is required for blood vessel contraction and dilation, muscle function, and nerve signaling.
Nonetheless, only 1% of the body’s calcium is used for these functions. The remaining 99% of the body’s calcium stores are in our bones and teeth.
Sources
We all know that dairy has dominated the marketing world for both calcium and vitamin D for quite some time.
Then again, with the increasing popularity of plant-based eating, there are plenty of non-dairy options for you to get your calcium and vitamin D requirements. Table 6 provides a list of calcium-rich foods.
If you are a milk lover, read this previous post about choosing milk for kidney disease here!
Table 6. Food sources of calcium
| Food | Milligrams (mg) per serving |
| Yogurt, plain, lowfat, 8 ounces | 415 |
| Orange juice, calcium fortified, 1 cup | 349 |
| Soymilk, calcium fortified, 1 cup | 299 |
| Milk, nonfat, 1 cup | 299 |
| Tofu, firm, made with calcium sulfate, ½ cup | 253 |
| Chia seeds, 1 tablespoon | 76 |
Forms of Calcium
The two main forms of calcium in supplements are calcium carbonate and calcium citrate. If you are taking a supplement containing calcium carbonate, it is best to take it with food to ensure maximum absorption as it does better with more stomach acid present.
Calcium citrate is best used for people with inflammatory bowel disease and people who don’t produce stomach acid.
Calcium, Kidneys, and Renal Hyperparathyroidism
If you, like many CKD patients, are living with renal hyperparathyroidism, you might be asking yourself how your kidneys have anything to do with it. It can be hard to understand the connection between the types of hyperparathyroidism and how they have anything to do with your kidneys at all.
You can think of your parathyroid hormone (PTH) as the director that tells your body to break down your bone tissue. This is a normal and healthy part of bone reformation when levels are in good range. However, too much of a good thing can quickly become a not-so-good thing.
When there is too much PTH being released, your blood calcium and phosphorus levels increase, which can lead to hypercalcemia. Signs and symptoms of hypercalcemia include nausea, vomiting, increased thirst, muscle weakness or twitches, and bone pain.
Next, let’s cover the two different types of hyperparathyroidism and how they can occur from kidney disease.
Types of Hyperparathyroidism
| Type | Cause | Treatment |
| Secondary Hyperparathyroidism | Phosphate build-up in the body and reduced vitamin D synthesis due to reduced kidney function. This leads to hypocalcemia (low levels of calcium) and in response, the body increases the amount of PTH released. | Low phosphorus diet, phosphate binders, vitamin D analogs, and/or calcimimetics |
| Tertiary Hyperparathyroidism | When secondary hyperparathyroidism is left untreated, mostly due to high calcium levels, it can develop into tertiary. It is also thought to be the result of parathyroid hyperplasia that causes the parathyroid glands to enlarge. | Same treatment as secondary, but surgical treatment may also be considered. |
It is recommended by the National Kidney Foundation that all patients with CKD progressive stage 3 should be screened for renal hyperparathyroidism by getting a baseline test done for PTH, calcium and phosphorus and re-evaluate every 6-12 months.
For CKD stage 4 patients, measure PTH every 6-12 months and calcium & phosphorus every 3-6 months.
For CKD stage 5 patients, measure PTH every 3-6 months and calcium & phosphorus every 1-3 months.
Talk with your doctor about setting up a screening and management plan for you to help prevent renal hyperparathyroidism.
Drug-Nutrient Interactions with Calcium
Calcium supplements and kidney disease can affect the way some medications work. It decreases the absorption of the following:
- Bisphosphonates (to treat osteoporosis)
- Select antibiotics (fluoroquinolone and tetracycline)
- Levothyroxine (to treat hypothyroidism)
- Phenytoin (anticonvulsant)
- Tiludronate disodium (to treat Paget’s disease)
If you are taking thiazide diuretics, they can interact with calcium supplements and increase your risk of hypercalcemia and hypercalciuria. Talk with your doctor about whether or not taking supplements is appropriate for you.
Recommended Intake and Deficiency
The daily recommended intake for calcium for men and women 19-50 years old is 1,000mg.
For men 51-70 years, this amount remains the same while it increases for women of the same age to 1,200mg. The RDA for both men and women ages 71 and up is 1,200mg.
Calcium deficiency, or hypocalcemia, is typically the result of medical problems or taking certain medications, such as loop diuretics. Renal failure and surgical removal of the stomach are also common causes for hypocalcemia.
Osteopenia is considered the mid-way point between hypocalcemia and osteoporosis. In this stage, the bones are beginning to weaken. If left untreated, osteopenia can turn into osteoporosis.
Osteoporosis is perhaps the most well-known risk of having low calcium levels, otherwise known as having porous and very fragile bones. Supplementation with calcium and vitamin D has been shown to prevent the development of osteoporosis.
Signs and symptoms of calcium deficiency include numbness and tingling of fingers, muscle cramps, convulsions, lethargy, poor appetite, and irregular heart rhythms.
Tolerable Upper Level Intake
Having excessive calcium in the body can result in renal insufficiency and vascular and soft tissue calcification. It can also cause constipation and it is suspected to interfere with iron and zinc absorption.
The tolerable upper level intake for men and women 19-50 years old is 2,500mg and is 2,000mg for those 51 and older.
Why is calcium important for kidney disease?
The kidneys are largely responsible for mineral balance in the body. When they are not at full functioning capacity, imbalances often emerge.
There have been a handful of studies done to try to understand calcium and kidney disease. That is to say, researchers are actively trying to find the correct calcium supplementation dose for CKD patients to keep them in a neutral balance.
Recent studies show that a calcium intake near the recommended daily allowance results in a neutral calcium balance.
In the case that you simultaneously have low calcium levels and high phosphorus levels, a calcium-based phosphate binder may be prescribed to you. Although, these binders are becoming less popular due to recent research showing accelerated vascular calcification in patients taking such binders.
There is a lot of talk on the effects calcium consumption has on developing kidney stones. With so much information out there, it can be hard to get an understanding of it all. You can read this previous post on how to prevent kidney stones if you need more clarification on the influence calcium has in kidney stone formation.
Nevertheless, it is important to note that everyone’s needs vary and it is important to talk to your doctor about whether or not supplements and/or certain phosphate binders may benefit you.
Zinc
Function
Zinc is popularly known for its immune boosting properties and can be found in many over-the-counter cold medicines. In addition to its role in immune function, zinc also aids in protein synthesis, wound healing, and DNA synthesis.
Sources
Red meat, poultry and certain seafoods provide most of the zinc in the average American diet. Although, there are many plant-based sources as well that can easily fit into your kidney lifestyle diet. See the table below for more food sources of zinc.
Table 7. Food sources of zinc
| Food | Milligrams (mg) per serving |
| Oysters, cooked, breaded and fried, 3 ounces | 74 |
| Beef chuck roast, braised, 3 ounces | 7 |
| Lobster, cooked, 3 ounces | 3.4 |
| Baked beans, canned, ½ cup | 2.9 |
| Breakfast cereal, fortified with 25% of the daily value for zinc, 1 serving | 2.8 |
| Pumpkin seeds, dried, 1 ounce | 2.2 |
| Cashews, dry roasted, 1 ounce | 1.6 |
| Chickpeas, cooked, ½ cup | 1.3 |
Forms of Zinc
Popular forms of zinc that can be found in supplements include zinc gluconate, zinc sulfate, and zinc acetate. However, there are no known studies that have researched the difference in absorption rates between these forms.
Drug-Nutrient Interactions with Zinc
Taking zinc supplements could have some effect on certain medications, including diuretics. See the list below for some examples.
- Antibiotics (quinolone and tetracycline type)
- Penicillamine
- Thiazide diuretics
Zinc is also known to interact with copper by affecting the absorption rate and, in high doses, can decrease copper levels in the body.
Recommended Intake and Deficiency
The daily recommended intake of zinc for men 14 years and older is 11mg. For women aged 14-18 years, the recommendation is 9mg and decreases to 8mg for women 19 years and older.
Most people in the US get an adequate amount of zinc in their diet, but the elderly population is of higher concern as 35% to 45% of adults 60 years and older do not meet the daily recommended amount.
Mild to moderate zinc deficiencies can result in growth retardation, loss of appetite, and impaired immune function.
However, more severe deficiencies can cause hair loss, diarrhea, hormone imbalances, weight loss, delayed wound healing, and taste abnormalities.
Tolerable Upper Level Intake
Toxicity from zinc from short-term excessive intake can result in nausea, vomiting, loss of appetite, diarrhea, and headaches.
However, long-term overconsumption of zinc can result in low copper status and altered iron function.
The tolerable upper level intake for zinc is 34mg for men and women 14-18 years old and 40mg for anyone over the age of nineteen.
Why is zinc important for kidney disease?
Studies have suggested that 40% to 78% of CKD patients experience low levels of zinc. It is thought that one of the main causes is because many foods rich in zinc are the same foods that CKD patients have to restrict. Hemodialysis also allows for excess zinc to be excreted during the filtration process.
However, there is some evidence that shows an increase in zinc levels in CKD patients has a positive effect on various inflammatory markers.
If you are wondering about your zinc status, you can talk to your doctor about getting a micronutrient panel done to see where your levels are at for zinc and other vitamins. Always consult your doctor before changing or starting a new supplement routine.
Potassium
Function
Potassium plays a very important role in fluid balance in every cell of the body. It also plays a role in nerve signaling, heart rhythm and muscle contraction.
Sources
Potassium can be found in both plant and animal based foods. The best sources include fruits, vegetables, and whole wheat and whole grain products (when compared to process grains).
A list of food sources for potassium can be found in Table 7.
Table 7. Food sources of potassium
| Food | Milligrams (mg) per serving |
| Apricots, dried, ½ cup | 1,101 |
| Lentils, cooked, 1 cup | 731 |
| Squash, acorn, mashed, 1 cup | 644 |
| Potato, baked, flesh only, 1 medium | 610 |
| Kidney beans, canned, 1 cup | 607 |
| Orange juice, 1 cup | 496 |
| Banana, 1 medium | 422 |
| Molasses, 1 tablespoon | 308 |
| Apple, with skin, 1 medium | 195 |
| Rice, brown, medium-grain, cooked, 1 cup | 154 |
Forms of Potassium
Potassium is usually included in supplements as potassium chloride, but other forms such as potassium citrate, phosphate, aspartate, bicarbonate, and gluconate may also be used.
Studies have found that humans absorb 94% of potassium gluconate from supplements, which is about the same amount of potassium you would absorb from potatoes, for example.
It is unlikely that you will need to look for a potassium supplement yourself as someone with CKD, but understanding how much potassium you are absorbing is still valuable information to know. However, research on the absorption rate of other forms are not yet available.
Drug-Nutrient Interactions with Potassium
There are several types of medications that potassium is known to interact with. A few examples are listed below.
- ACE Inhibitors and angiotensin blockers (ARBs)
- Potassium sparing diuretics
- Loop and thiazide diuretics
Potassium sparing diuretics such as amiloride and spironolactone reduce the amount of potassium excreted in the urine and can cause hyperkalemia, aka high levels of potassium.
Loop and thiazide diuretics such as furosemide, bumetanide, chlorothiazide and metolazone increases the amount of potassium excrete in the urine and can cause hypokalemia, aka low levels of potassium.
Recommended Intake and Deficiency
The adequate intake for potassium for men 19 years and older is 3,400mg per day. For women 19 years and older, 2,600mg per day is suggested.
These suggestions do not apply to individuals with kidney disease due to impaired potassium excretion. Therefore, speak with your doctor to learn more about what your individual needs are based on your condition. If you’ve been told to follow a low-potassium diet, this article may be very useful to you!
Potassium deficiency can increase blood pressure, kidney stone risk, and salt sensitivity. When severe, a deficiency is labeled as hypokalemia.
Mild hypokalemia can cause constipation, fatigue, muscle weakness, and discomfort. When the deficiency becomes moderate to severe, it can also result in encephalopathy in kidney patients, causing damage to the brain.
Low levels of potassium are usually the result of a disease state, such as CKD, or of a medication like certain diuretics. This is why it’s important to communicate with your doctor so you understand how your treatment may affect you and what precautions to take.
Tolerable Upper Level intake
For the average healthy person, excess potassium consumption is not of much concern. In contrast, for the average CKD patient, too much potassium can have serious health implications.
To note, the consequences of severe hyperkalemia include muscle weakness, paralysis, heart palpitations, and cardiac arrhythmias.
There is currently no set standard for potassium intake for the general population, but it is important that as someone with kidney disease, you talk to your doctor about your personal limits.
Why is potassium important for kidney disease?
Above all, Potassium needs vary greatly from one CKD patient to the next. Factors influencing your personal requirements include kidney function level, medications, and whether or not you are on dialysis and what type.
In the average healthy person, the kidneys are normally responsible for filtering out any excess potassium in our bodies so that our levels stay in a healthy range of 3.5-5mg/dL.
As the kidneys become less functional, they lose this filtration ability. Despite this, it is important to know that you should only restrict your potassium intake if your doctor has told you to do so.
If you unnecessarily limit your potassium intake, you can increase your risk of developing hypokalemia, which can lead to more serious health implications like abnormal heart rhythms.
Fruits and vegetables are an important part of anyone’s diet, but CKD patients should be aware of what they are consuming. Talk to your doctor about what your personal needs are according to your labs.
Here’s a great article if you are looking for more information about a low potassium diet.
Sodium
Function
Sodium is an essential nutrient that helps maintain the water balance in our bodies. It also helps nerve cell function and is needed for muscle contraction.
Sources
Animal based foods tend to have more naturally occurring sodium compared to fruits and vegetables. Regardless, the majority of sodium in the American diet comes from processed foods like deli meats, breads, dairy products, frozen meals, etc.
See Table 8 for a list of food sources of sodium.
Table 8. Food sources of sodium
| Food | Milligrams (mg) per serving |
| Bagel, 1 medium, ½ bagel | 288 |
| Tomatoes, canned, ½ cup | 236 |
| Bread, whole wheat, commercial, 1 slice | 213 |
| Eggs, whole, cooked, 2 large eggs | 125 |
| Chickpeas, canned, drained, rinsed, ¾ cup | 225 |
| Mustard, yellow, 1 tablespoon | 174 |
| Peanut butter, 2 tablespoons | 139 |
| Chickpeas, no salt added, canned, ¾ cup | 7 |
| Cashews, unsalted, ¼ cup | 6 |
Forms of Sodium
Sodium can often be found in its most stable form of sodium chloride in supplements that also contain other vitamins & minerals and is sold as an electrolyte complex. Sodium is an electrolyte, and we need to pay close attention to electrolytes and kidney disease.
However, if you see sodium ascorbate at the store, don’t be fooled by the first half of the name. It’s actually just a different form of vitamin C that is paired with sodium! This combination makes the vitamin C less acidic for those sensitive to acidic foods.
Drug-Nutrient Interactions with Sodium
Studies suggest that patients on antihypertensive drugs would benefit from moderate sodium restriction.
Recommended Intake and Deficiency
The daily value for sodium for the general population is less than 2,300mg per day. This is fairly close to the current recommendation for CKD patients of 2,000mg per day. So why is it that someone with full functioning kidneys is still suggested to have roughly the same sodium goal?
Well, when you consider that the average American consumes closer to 3,400mg of sodium each day it puts things into perspective. The majority of the population is so used to overconsuming sodium that limiting it by over 1,000mg is the bare minimum needed to take the average person down from high to low risk for medical conditions like hypertension.
Above all, remember that it is important to set consumption limits with your doctor as your diet plan should be individualized and tailored to you and the state of your condition.
Sodium deficiency (hyponatremia) is rare and typically only occurs when accompanied with another existing medical condition, such as chronic diarrhea, sodium-losing kidneys, gastric cancer, etc.
Tolerable Upper Level Intake
High intake of sodium case reports have shown that rapid ingestion of salt in liquid solution can have fatal outcomes.
Hypernatremia is defined by the sodium concentration in your blood exceeding 145meq/L. Signs and symptoms include thirst, fatigue, restlessness, increased heart rate, and decreased urine production.
Why Is Sodium Important for Kidney Disease?
Usually the amount of sodium in the body is tightly regulated by the kidneys. Unfortunately, in the case of chronic kidney disease, the control must lie with the patient.
Sodium is essential whether you have CKD or not. High sodium intake has long been known to cause an increase in blood pressure. This, of course, should be a worry to everyone but especially to those with kidney disease.
Kidneys are largely responsible for controlling your blood pressure, and when dealing with CKD this capability is diminished. Adding a high amount of sodium in the diet to this already existing issue only worsens it, and can eventually lead to hypertension.
Excess sodium intake with CKD has also been shown to increase proteinuria (excretion of protein in urine), kidney blood flow, and even prevents anti-hypertensive agents from properly working.
Reducing sodium intake has shown vast health improvements in many studies such as decreased proteinuria by 30% and blood pressure, reducing your risk for developing hypertension.
The current recommendation for sodium limitation for CKD patients is 2,000mg a day. However, remember to always take the advice of your medical provider as everyone’s condition varies greatly.
If you are having trouble finding low-sodium snack ideas, you can find some suggestions here in a previous post!
How to Choose Minerals and Electrolytes for Kidneys
My Recommendations
It’s easy to become overwhelmed by which minerals for kidneys to get, whether it’s online and in stores. If you’re looking for a multivitamin that has everything you need all in one, you can find my preferred brands on my Amazon shop* for reputable brands that I trust.
For those in the United States, I have a Fullscript dispensary* in which you can receive 15% off of your supplement order!
These multivitamins contain vitamins and minerals in appropriate doses for many CKD patients, however, remember to always consult with your medical provider before starting a new supplement routine.
Third Party Verification
The FDA is not responsible for reviewing the safety and effectiveness of supplements before they are marketed. However, all supplement manufacturers are required to follow Current Good Manufacturing Practices which sets certain standards for products all across the board.
Even with these standards in place, looking for a third party verification label is a good way to ensure you know what you are buying. This means that a separate, non-affiliated company comes to verify the potency and practices used to create the product at the manufacturing site.
Below are some easy-to-spot images of popular third-party testers that you can look for when purchasing supplements.
Looking for Additives
Additionally, if you follow a strict vegetarian or vegan diet, you will also want to look for the type of coating a supplement has. Many use animal-derived ingredients for their capsules.
Supplements also may also have added sweeteners or come in a “gummy” form that you may want to avoid.
Summary
In conclusion, minerals provide a wide range of benefits whether they are coming from food or supplement sources. They are vital nutrients that help your body carry out necessary bodily functions.
Many people with kidney problems may find themselves deficient in certain minerals, like iron, as the main dietary source comes from animal-based foods, something that is often restricted in the diet for those with CKD.
The three minerals with the largest influence on kidney health is phosphorus, sodium, and potassium. However, please consult your doctor to find out your specific needs for minerals and electrolytes for kidneys.
You could start the conversation on electrolytes and kidney disease with your doctor by asking about getting a micronutrient test done, like Spectracell, to see what you are deficient in.
There are a handful of multivitamins formulated with CKD patients in mind, but you can find my personal recommendations here and you will receive 15% off your order!

Thanks for the great information. Appreciate what you and James do for all of us looking to stay on top of information and diet, etc.
Thank you for the kind words, Karen! 💚
I can only second what Karen Strozewski wrote. My wife was diagnosed with stage 5 just a few months ago. She had to go in the hospital’s emergency room for different reasons. That’s when the blood and urine samples, taken at the ER, showed only 15 percent function left.
We came across your website and all the information, and this is just what we needed. Thanks for doing all the work and detailed information.
Thanks so much! We are honored to be a resource for you and your wife. Feel free to check out our other articles, including our stage 5 guide.