There are several situations where a fluid restriction in CKD (chronic kidney disease) can help. Whether it’s stage 3, dialysis patients, or anywhere before or in between, a fluid restriction can become critical when caring for kidney health. But how much fluid does that mean? What happens if you drink too much? Is there a risk for dehydration? This article will cover fluid restrictions in CKD.
*This article contains clearly identified affiliate links. We may earn a very small percent commission based on sales made through the link at no expense to you. We only recommend products and services that we use ourselves and/or use with clients. Thank you for supporting our business!
Table of Contents
What is a fluid restriction?
A fluid restriction is a medically-directed order in which a person needs to limit liquid or fluid intake to prevent complications from an excessive fluid collection in the body.
Fluid overload is a term used that can indicate the need for a fluid restriction in CKD. This simply means there is more fluid in the body than there should be.
What are the symptoms of having too much fluid with kidney disease?
Symptoms of too much fluid can vary quite significantly. In many cases, symptoms won’t be noticed until later, as the body adapts to the situation.
Examples of fluid overload symptoms may include:
- Swelling at the feet, ankles, hands, even face
- Rapid weight gain
- Headache
- Cramping
- Bloating
- Abdominal pain or discomfort
- Shortness of breath
- Hyponatremia (low sodium levels in the blood)
- High blood pressure
However, not all of these symptoms need to be present to indicate fluid overload. In fact, some do not feel any symptoms at all.
A person with chronic kidney disease caused by high blood pressure, for example, may not realize their high blood pressure is also caused by fluid overload. But not everyone with high blood pressure will have a fluid restriction.
It’s important to speak with your doctor and dietitian about your fluid guidelines to determine if you need to be on a fluid restriction.
What happens if I drink too much water when I have kidney disease?
If you have a fluid restriction advised by your doctor and healthcare team, too much fluid can be extremely hard on your body.
Too much water can cause sodium levels to drop below the normal range and cause hyponatremia.
This can lead to severe health problems. Other electrolytes, such as potassium, may also come out of range and cause further severe health complications.
Heart failure is one of the leading causes of death in chronic kidney disease, in part related to efforts of fluid balance.
Dehydration vs Fluid Restriction
If following a medically necessary fluid restriction, dehydration is unlikely. This is because the doctor has found that too much fluid is likely to cause more health problems.
However, if you do not drink enough fluids even while on a fluid restriction there is a risk of becoming dehydrated.
Daily weight measurements can be very helpful when monitoring fluid balance on a fluid restriction. More on that later on in this article.
What counts as a fluid in a fluid restriction?
Both foods and beverages will count in a fluid restriction. Any type of fluid will be counted. If it is liquid at room temperature, it is considered a fluid.
The most common liquids include:
- Water (flat, filtered, tap, carbonated, flavored, etc)
- Coffee
- Tea
- Lemonade
- Milk
- Juice
- Alcohol
- Soft drinks
- Energy drinks
Besides beverages, any foods that have liquid will also need to be included in a fluid restriction. Examples include:
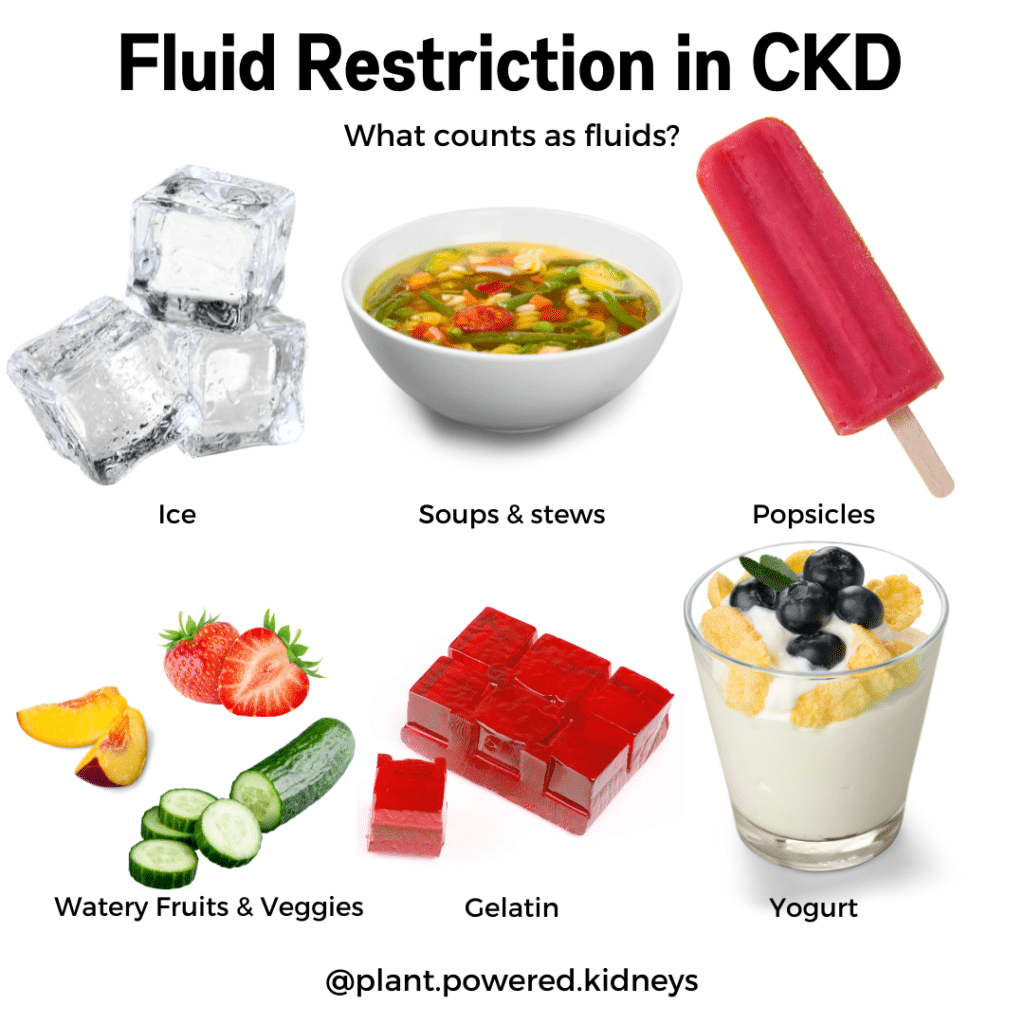
- Ice
- Soup
- Stew
- Yogurt
- Ice cream
- Gelatin
- Sauces
- Watery fruits and vegetables such as watermelon, cucumber, strawberries, cantaloupe, and peaches
Examples of fluid amounts in different food items
| Food Item (serving size) | Volume of water (mL) |
|---|---|
| Ice (crushed, 1 cup) | 120 |
| Ice cube (1 oz) | 30 |
| 1 can soda (12 oz) | 332 |
| Gelatin (1 cup) | 200 |
| Popsicle | 45 |
| Ice cream/sherbet (1 cup) | 127 |
| Yogurt (1 cup) | 182 |
| Peaches, canned (1 cup) | 218 |
| Grapes (1 cup) | 120 |
| Watermelon (1 cup) | 140 |
| Apple (1 medium) | 171 |
Even foods can count towards a fluid restriction. This is where portions are important with your renal diet and fluid restriction or other guidelines.
Next is a fluid conversion table. This can help with different fluid restriction guidelines provided.
Fluid Conversion Table
| 1 gallon | 128 ounces / 16 cups | 3785 milliliters (mL) |
| 1/2 gallon | 64 ounces / 8 cups | 1893 mL |
| 1 quart | 32 ounces / 4 cups | 960 mL |
| 2 1/2 cups | 20 ounces | 600 mL |
| 1 pint | 16 ounces / 2 cups | 480 mL |
| 1 cup | 8 ounces | 240 mL |
| 3/4 cup | 6 ounces | 180 mL |
| 2/3 cup | 5 1/3 ounces | 158 mL |
| 1/2 cup | 4 ounces | 120 mL |
| 1/3 cup | 2 2/3 ounces | 80 mL |
| 1/4 cup | 2 ounces | 60 mL |
| 1 Tablespoon | 1/2 ounce | 15 mL |
| 1 teaspoon | 1/6 ounce | 5 mL |
For example, a 1-liter fluid restriction is approximately 4 cups or 1 quart of water. A half-gallon fluid restriction is 8 cups or 1,893 milliliters per day.
Do I need to be on a fluid restriction with kidney disease?
Kidney disease is a chronic illness with many stages and causes. Each person will have their own diet and fluid needs.
Your primary doctor or kidney specialist will be able to help you understand if you need to be on any fluid restriction. Remember a diagnosis and stage of CKD can only come from a healthcare provider.
Stage 3 Kidney Disease Water Intake (and earlier stages)
In general, there is no fluid restriction in CKD stage 3. A bigger focus when it comes to fluid management with early stages of CKD starts with a focus on sodium restriction.
Stages 1 and 2 of chronic kidney disease also do not typically have a fluid restriction. Fluids are more often encouraged to be consumed according to thirst.
However, there may be a need for a fluid restriction if a person with stage 1-3 CKD also has congestive heart failure.
It is extremely important to discuss individual healthcare needs with your own physician.
Stage 4 Kidney Disease Water Intake
Many with stage 4 CKD will start to have diet restrictions at this stage. Some restrictions may include a low phosphorus diet, a low protein diet, a low potassium diet, and a fluid restriction.
However, it is not a guarantee that all will be needed.
Discuss individual dietary and fluid restriction guidelines with a personal healthcare team. They know the history, labs, and situation of an individual to appropriately determine a fluid restriction.
Stage 5 Kidney Disease Water Intake
Stage 5 is considered to be a glomerular filtration rate (GFR) of below 15. This is also the period at which a person qualifies for dialysis and/or kidney transplantation.
A fluid restriction will likely be addressed by the nephrologist at this point in kidney disease.
Water and fluid intake is often restricted for stage 5 due to the limited kidney function remaining. At this stage, a fluid restriction may be anywhere from 1 liter to 2+ liters per day.
The water intake for stage 5 will be calculated based on the individual’s age, size, activity, labs, and health conditions. It is not just because of a certain stage of kidney disease.
What’s the recommended fluid intake for dialysis patients?
Dialysis patients are the ones most likely to benefit from a fluid restriction.
The recommended fluid intake in dialysis can be anywhere from one to three liters of fluid per day, depending on the dialysis modality, residual renal function, and individual fluid needs.
In the United States, every person on dialysis will be seen by a dietitian. Your dialysis dietitian will go over your food and fluid intake and needs to help guide you on if you’re getting enough, too much, or not enough fluid.
If you have any questions about your fluid restriction on dialysis, speak with your dietitian first.
When Not to Have a Fluid Restriction
There are certain cases, even with kidney disease when more fluids are important.
Whether it’s more fluids or a fluid restriction in CKD, it’s an important conversation to have with your doctor and healthcare team.
Increasing fluid intake just because you have kidney disease may not be helpful, but there are some cases in which more fluids are important.
Polycystic Kidney Disease
Polycystic Kidney Disease, aka PKD or ADPKD, generally requires more fluids. This is especially important in the earlier stages of diagnosis of PKD. Fluid intake for polycystic kidney disease can be up to 3 liters of fluid per day to help reduce the amount of vasopressin in your body.
Kidney Stones
If you have kidney stones, your doctor may be telling you to drink more fluids to prevent kidney stone formation.
Kidney stones are produced with minerals collected in the kidneys or ureters and create mineral deposits.
By drinking more fluids, there is continuous flushing of the kidneys and ureters. This limits the opportunity for these minerals to collect and form stones.
It’s still important to know your fluid goals from your healthcare provider so you have a target amount to aim for that is relevant to your own needs.
Kidney Disease
As discussed above, just having chronic kidney disease does not mean a fluid restriction is necessary or even helpful.
In certain cases, drinking enough water can be very important in preserving kidney function.
This is why it is very important to speak with your nephrologist, doctor, and/or dietitian before limiting fluids.
Examples of fluid restriction in CKD
Below are some examples of what a day would look like with different fluid restrictions.
Again, it’s important to only limit fluids if instructed by your doctor. Following a fluid restriction without medical direction can result in dehydration and electrolyte imbalances, among other complications.
Sample day with 1 Liter fluid restriction
Breakfast: ½ cup oats cooked with 8 oz (1 cup) water (240 ml) + 8 oz black coffee (240 mL)
Snack: Whole grain crackers with peanut butter + 8 oz of water (240 ml)
Lunch: 1 cup kale salad with walnuts and feta
Snack: Dry roasted edamame + 8 oz of water (240 ml)
Dinner: Spaghetti Squash with 1 oz Marinara Sauce (30 mL) + chickpeas
Total fluids: 990 mL
Sample day with 1.5 Liter fluid restriction
Breakfast: ½ cup oats cooked with 8 oz (1 cup) water (240 ml) + ½ cup strawberries (60 mL) + 8 oz black coffee (240 mL)
Snack: Whole grain crackers with peanut butter + 8 oz water (240 mL)
Lunch: 1 cup kale salad with walnuts, feta and ½ cup of grapes (60 mL)
Snack: 1 cup almond yogurt (182 mL) + ½ cup blueberries (60 mL) + 1 glass of water (240 ml)
Dinner: Spaghetti squash with 2 oz marinara sauce (60 mL) + chickpeas
Dessert: ½ cup ice cream (64 mL)
Total fluids: 1,446 mL
Sample day with 2 Liter fluid restriction
Breakfast: ½ cup oats cooked with 8 oz (1 cup) water (240 ml) +½ cup strawberries (60 mL) + 8oz black coffee (240 mL)
Snack: Whole grain crackers with peanut butter + 8oz water (240 mL)
Lunch: 1 cup kale salad with walnuts, feta, 1 cup chopped tomatoes (120 mL) and 1 cup of grapes (120 mL) + 8 oz water (240 mL)
Snack: 1 cup almond yogurt (182 mL) + 1 cup blueberries (120 mL) + 1 glass of water (240 ml)
Dinner: Spaghetti squash with 3oz Marinara Sauce (90 mL) + chickpeas
Dessert: ½ cup ice cream (64 mL)
Total fluids: 1,956 mL
Medications prescribed for fluid restrictions
If you are struggling with your fluid balance, your doctor may prescribe a diuretic. Diuretics help trigger the body to make more urine and release more fluids.
Diuretics are to only be taken under medical supervision.
Examples of common diuretics include:
- Thiazides
- Chlorothiazide
- Chlorthalidone
- Hydrochlorothiazide
- Indapamide
- Metolazone
- Loop diuretics
- Bumetanide
- Furosemide
- Torsemide
- Potassium-sparing diuretics
- Amiloride
- Triamterene
- Spironolactone
Since diuretics help remove fluid from the body, they may also impact potassium levels. Some diuretics can increase potassium and some can decrease potassium.
Because of this and other reasons described above, diuretics are medically prescribed and monitored. For any concerns regarding medications, speak with the prescribing physician.
Tips to Track a Fluid Restriction in CKD
If you have to restrict your fluid intake, you may find a log to be helpful. Here are some tips when it comes to successfully tracking your fluid balance.
Use a food and fluid journal
As mentioned above, many foods have high water content and can make a difference in how much fluid you’re actually consuming.
By using a food and fluid journal, you’ll have a better idea of what you’re taking in.
Your doctor and dietitian will also be able to give you better recommendations if you have a detailed log to provide.
We highly recommend Cronometer. They offer a free plan, which does include tracking fluids and sodium.
Here is our Cronometer affiliate link*, which you can use for their free plan or get 10% off their Gold Plan to track additional values such as PRAL, print and share reports with your doctor or dietitian, and customize nutritional goals.
Weigh regularly
It’s very important to consistently track weight when it comes to monitoring fluid balance. The body is made up of up to 60% water, but that can change significantly if the body cannot balance fluids on its own.
Some scales can even give you an estimate of your water percentage along with your weight. We use and recommend a bluetooth-enabled scale, like this FitIndex Scale*.
It will check the water percentage as well as overall weight trends. Both of these values can be helpful when shared with your doctor and dietitian.
Consistent tracking is a great tool to monitor any fluid balance trends (rather than the exact numbers).
Weigh around the same time of day each day (or as directed by your healthcare provider) and in the same clothing for the best accuracy.
Check your blood pressure consistently
An arm blood pressure cuff with monitor is a great way to check blood pressure at home. We recommend this Omicron Gold Cuff and Monitor*, which stores up to 14 blood pressure readings.
It is incredibly helpful to track blood pressure consistently since fluid balance can also impact blood pressure.
Adding blood pressure details to a fluid log, along with weight, can give the doctor a great picture of how fluid balance looks day-to-day.
Tips to following a fluid restriction when you’re thirsty
Following a fluid restriction can be a challenge, but it often comes down to having a list of solutions to prevent yourself from getting too thirsty or overdoing it with your fluids.
Brush your teeth regularly
Good dental hygiene is important for kidney disease for many reasons, including controlling your thirst!
The recommendation is to brush two to three times daily after meals to keep your pearly whites and gums in top shape.
Suck on a lemon slice
This isn’t an insult- it’s actually a trick!
Even if you don’t have a lemon on hand, imagine this: biting into a big, juicy lemon wedge. Is your mouth watering yet?
Make flavored ice cubes
Create a tray of flavored ice cubes using fruit like berries, watermelon, cucumber, and yes, lemon!
While ice still counts as a part of your fluid restriction, it’s generally giving you about half of what you’d drink if it were just water.
For more tips, check out our article fluid restriction tip article here.
The main point For a fluid restriction in CKD
The ultimate goal when it comes to fluid restriction in CKD is to protect the body, the kidneys, and the heart from being overworked with excess fluid. This helps protect the heart and cardiovascular system from having to push more fluid through the body.
If instructed to limit fluids, ask for a goal amount of fluid from your doctor. Working privately with a dietitian can also help with managing your fluid restriction.
Using a food and fluid journal like Cronometer* can help make tracking easier, especially when it comes to tracking fluids from watery foods like cucumbers, strawberries, and peaches.
Keep up with routine medical appointments to check in on your progress. A fluid restriction in CKD can change, either increasing or decreasing fluid needs depending on health conditions, diet, labs, and medications.

![17+ Gift Ideas for Dialysis Patients [Dietitian-Recommended]](https://www.plantpoweredkidneys.com/wp-content/uploads/2020/11/17-Dietitian-Recommended-Gift-Ideas-for-Dialysis-Patients-Blog-Title.png)
Thanks Jen, this was a very insightful article on fluids. As one with Stage 2 CKD and KS it has always been confusing to hear the recommendation to drink more fluids so you make at least 2.5 liters of urine to reduce the risk of KS… Fluid overload has complications.
Yes, everyone is different, even in the same stages. I’m glad you found this article helpful! 🙂
Oh my lordy i drink way too much liquid probably why my feet are always swollen ,i have been only counting my water intake
That’s why it’s important to chat with your healthcare team about what is right for you! 🙂
Helps me to track my water consumption. Thanks for the good advice, Jen.
Candy
So happy to hear that, Candy! 🙂
When I was diagnosed stage four in 2009, my dietitian recommended 3 liters of water including other fluids. However, after my kidney recovered to stage 3 in two years, my nephrologist and dietitian reduced my fluid intake to two and half liters. I am following this since then and I do not have any problem with fluid intake. Thanks for the article which will be beneficial for those who have been suffering from kidney disease.
It’s always best to follow the guidelines set by your own healthcare team. Nice job!
Hi Jen, Thank you for the guidelines. My father has been diagnosed with Stage 3 CKD, GFR 39. He complains of bitter taste. It vanished when he reduced his water intake as advised by the nephrologist and now he drinks as per his thirst. But he again started to have it. Any advice?
Many thanks
Hi Poonam,
The only advice I can give here is to report it to the nephrologist for further evaluation. These are symptoms that should be evaluated!
Best of luck!!
I am have just gone from stage 3 to stage 4 CKD like to know your Nephrologist protocol that helped you?
Hi Ron, we recommend working privately with a dietitian to help slow the progression of CKD. Learn about our team of dietitians here.
What kind peanut butter you said I can’t remember the name of it
We generally recommend natural peanut butter that has just peanuts. 🙂
Whats the required amount of water intake is best for a person with stage 2 ckd of 84.6
That would be an individual guideline, which can only be provided by your healthcare team. But in general, early-stage CKD does not include a fluid restriction.
Well this is concerning. My husband is in hospital with UTI (and he has 30 GFR) they have been pumping him with 3 litres of IV fluid per day, but have him on liquid restriction simultaneously.
He gained 6kg in the past two days, I fear they are killing him (Hyperkalemia)-I’m not doctor but does this action make sense to you?
I’m sorry to hear that, Angela. We can’t comment about the treatment plan, but it’s always important to ask the healthcare team questions to get a good explanation. Sometimes all it takes is listening to why they’re doing something to help see the big picture. Wishing you both the best and I hope he’s well soon!
the link for the blood pressure cuff takes you to a page for a FITINDEX Bluetooth Body Fat Scale, Smart Wireless BMI Bathroom Weight Scale Body Composition Monitor Health Analyzer with Smartphone App for Body Weight, Fat, Water, BMI, BMR, Muscle Mass – White
Thank you so much for letting us know, Lisa. It’s been corrected. 😊
I am diagnosed as CKD-4 which came quickly in 6 months without proper diagnose by my NEPHROLOGIST. I have too much swelling on the foot , irritation of the skin and scratching
What can I do ? Looks like I am the first kidney patient with such symptoms and Doctors are pointing figures
Sorry, you’re having a rough time.
You are not the 1st person with CKD to experience these symptoms.
Check out our blog on itching and CKD.
My husband: age 79 has had increasing levels of the usual kidney function labs. He also has lessening hemoglobin and from the work I did professionally, I am suspicious of erythropoiten deficiency. I am not an MD, of course. The lastest labs were ‘evaluated’ by a NP who told him to greatly increase his water intake. We are not comfortable with this direction. I do not know what ‘stage’ he would considered to be…low, I know.
I mentioned the ‘erythropoitin’ matter about two years to his Doc, who told me he has only seen the ‘erythropoiten’ issue in someone who has very severe CKD. Somehow we need further input on his water intake. He already has continence and abrupt flow, etc. problems. Thanks
Thanks for sharing, Carolyn. There are frequent times we have seen labs to be altered due to hydration status, so it can be an important consideration. However, that’s not always the case, and it’s best to continue discussion with your healthteam. Asking your husband’s doctor for a referral to a dietitan can be a great way to get more details about his water intake & needs, as well as more diet recommendations with a personal lab review. Best of luck to you both! 💚