Chronic kidney disease (CKD) is a condition brought on by damage to the kidneys. There are 5 stages of kidney disease. If the kidneys go unprotected, additional damage occurs and the condition will worsen. Though stage 5 kidney disease is very serious, there is still a lot you can do to strengthen the kidneys. Read on to learn all about a diet for kidney disease stage 5 patients that are not on dialysis. This article will detail nutrition topics such as protein, potassium, sodium, and phosphorus in a stage 5 kidney disease diet.
Table of Contents
What Is Chronic Kidney Disease?
When healthy kidneys become damaged a condition known as chronic kidney disease (CKD) sets in.
This is a big problem for many Americans.
There are currently 37 million people who are suffering from CKD according to the National Kidney Foundation.
The 5 Stages of Kidney Disease
Before we cover stage 5 kidney disease we want to briefly go over the 5 stages of kidney disease to show how if no efforts are made to manage CKD, kidney function will quickly decline.
Kidney damage goes from a little to more severe if it progresses across each stage.
Stage 1 and 2 are mild with little change in function and no symptoms.
Stage 3 is right in the middle. It is considered not as bad as stages 4 and 5, but worse than stages 1 and 2.
This is when the condition is physically detected. In stage 3, the kidneys still have an adequate amount of function.
Learn more about stage 3 kidney disease in this post.
Stage 4 is when you really start to see severe damage. This is also when the discussion of diet changes and possible dialysis can start to happen.
Learn more about stage 4 kidney disease in this post.
So if you’re wondering what is end-stage renal disease, it is when stage five kicks in.
Stage 5 kidney disease is also known as end-stage kidney failure. About 85% of function is no longer available. Subsequently, they will begin to fail.
Unfortunately, 2 in 5 adults with severe kidney disease do not even realize they have it.
Only your healthcare physician or kidney specialist can diagnose and classify your stage of kidney disease using your blood test results.
Don’t be in despair if you are in stage 5 kidney disease and are only finding out. We will help give you information on what a stage 5 kidney disease diet can look like.
Nutrients to Monitor
To keep the kidneys functioning it is imperative to monitor certain nutrients during stage 5 kidney disease. They include the following:
- Sodium
- Calcium
- Phosphorus
- Potassium
- Magnesium
- Iron
- Fluid
- Protein
We will start by reviewing these nutrients and what to look for.
Be sure to discuss your labs and nutrients with your healthcare team. They will provide you with the most specific and personalized information.
The information below is to help get you set up on the right path to be informed and aware of your nutrients in chronic kidney disease.
Sodium
Sodium is an important nutrient to monitor. Our bodies will lower fluid levels to balance sodium. Sodium levels will also tell if your fluids are regulated.
Normal sodium levels should be 135 and 145 milliequivalents/liter (mEq/L). Having less than 135 is too little sodium and you will be in a hyponatremic state.
Sodium levels above 145 mEq/L show the body to be in hypernatremia with too much sodium in the blood.
High levels of sodium also occur due to dehydration. Alternatively, a test showing hypernatremia can be due to too much water intake before the blood test.
Hyponatremia is also a result of edema and fluid retention.
If your sodium levels are out of range ask your renal dietitian what dietary changes can improve sodium balance.
Calcium
Kidneys regulate calcium so monitoring this mineral will give you information on how you are managing your CKD. This can be done with a calcium blood test.
Calcium between between 8.5 and 10.5 mg/dL (4.3 to 5.3 mEq/L or 2.2 to 2.7 mmol/L) are normal. Lab ranges vary up to 0.5 mg/dL in either direction.
During stage 5 kidney disease calcium levels can get too high (hypercalcemia) and/or too low (hypocalcemia). When calcium gets out of whack they need to be continuously tested. Especially when people are getting therapy for problems with calcium, phosphorus, and/or PTH levels.
If you find you have calcium issues talk to your healthcare team about how to improve your levels.
Phosphorus
Phosphorus is regulated by the kidneys. Weakened kidneys cause elevations of this mineral. As a result, continuous monitoring of phosphorus is necessary during CKD.
For those with stage 5 kidney disease, phosphorus levels should between 3.5 and 5.5 mg/dL.
If diet cannot maintain phosphorus levels, phosphate binders may be needed. Consequently, this medication can cause elevated calcium. So this medication should not be taken without medical supervision.
Potassium
Healthy kidneys are needed to maintain normal potassium levels. Potassium levels that are too high or too low are very dangerous.
The normal level runs between 3.5 and 5.0 mEq/L.
Hyperkalemia is the technical term for high potassium levels in the blood. This occurs when levels are greater than or equal to 5.5 mEq/L.
Your doctor will address your potassium levels with you from your blood test results. You may be referred to a dietitian if you have high potassium levels.
Iron
Iron is a mineral that needs to be constantly monitored in people with stage 5 kidney disease. This is because iron deficiency is very common in CKD.
Iron should be between 60 to 170 mcg/dL. If your levels deviate from this you could have anemia or hepatitis.
It could also be due to a medication you are taking. Women with heavy menstrual periods will also have lower iron levels.
In addition, you should know that hemoglobin, ferritin, and transferrin saturation in the CBC panel will give a full picture of your iron status.
If your iron is out of range, talk with your healthcare team to find what could be the problem.
Fluid
During stage 5 kidney disease water intake and fluid levels need to be monitored.
Too much fluid indicates poor kidney function. Fluid restrictions are often mandated in this phase of the disease.
If you have a fluid restriction a renal RD can help you keep your fluid intake under control.
Foods to Limit or Avoid in a Stage 5 Kidney Disease Diet
The kidney failure diet may have more restrictions but it can be helpful to preserve remaining kidney function.
In this section, we will discuss some of the foods and food groups that may need to be limited or avoided in certain circumstances.
This will not mean that just because you have stage 5 kidney disease you need to avoid these foods. So read closely to understand the situations related to stage 5 that could result in removing these foods.
Sugary Foods and Drinks
Diabetes is often the main cause of stage 5 kidney disease. So a big key to managing CKD is getting your diabetes under control.
Knowing that sugary foods and drinks elevate blood sugar, these foods should be avoided during stage 5 kidney disease when blood sugar control is a concern.
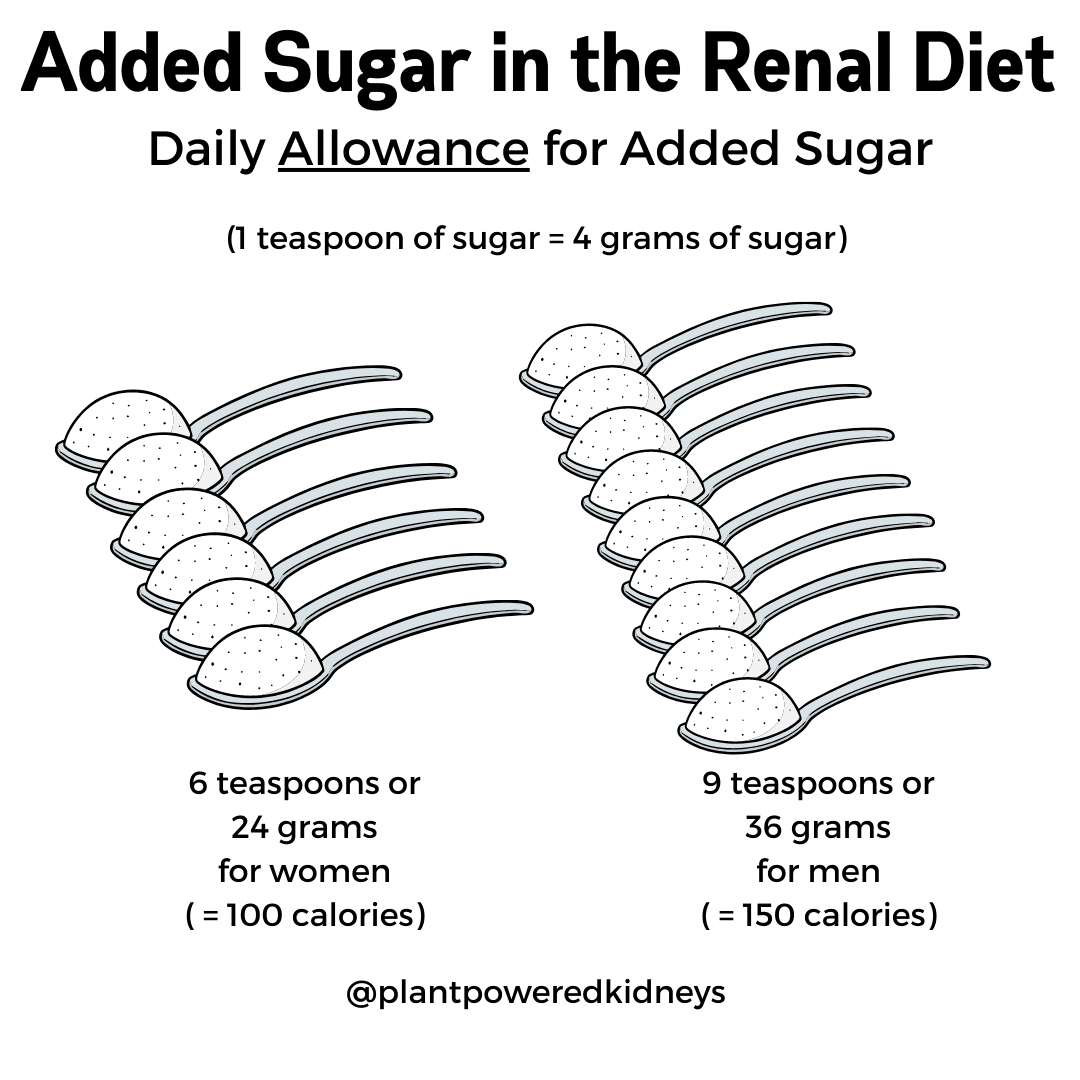
Aim for no more than 10% of your calories from added sugar.
For example, if you have a 2,000 calorie diet you want less than 200 calories from added sugar.
Added sugar is found in processed foods, drinks, and even some healthy foods. Juices have a lot of sugar and may need to be eliminated or limited.
Simple sugars increase the risk of type 2 diabetes and provide no nutrition. The following foods should be limited or avoided
- White bread
- White pasta
- Pastries
- Soda
- Candy
Refined Carbohydrates
Certain carbohydrates can send your blood sugar sky high and further weaken the kidneys.
The following refined carbohydrates should be limited when you have stage 5 kidney disease
- Sugar
- White bread
- Pizza dough
- Pasta
- Pastries
- White flour
- White rice
- Sweets
- Desserts
- Breakfast cereals
- Sugary beverages
If you have carbohydrate restrictions ask your dietitian how to meet your carbohydrate needs with a healthy diet.
Learn more about the best foods for a renal diabetic diet here.
High Sodium Foods
The more sodium you have in your diet the higher your blood pressure will be. This is because the kidneys cannot excrete excess sodium in the blood.
The easiest way to lower your blood pressure is to cut back on your sodium. This also will prevent further damage to the kidneys.
Sodium intake recommendations are about 2,000 mg a day. Anyone with high blood pressure should decrease this to about 1,500 mg.
High sodium foods need to be avoided in those with stage 5 kidney disease. This can preserve kidney health, lower blood pressure, and prevent fluid imbalances.
High sodium foods to avoid include
- Table, sea, and garlic salt
- Soy sauce
- Bottled sauces like Teriyaki sauce
- Canned and dehydrated foods and soups
- Frozen dinners that are not listed as “low sodium”
- Processed meats like ham, bacon, hot dogs, sausage, and deli meats
- Take out, restaurant, and fast food
For a full list of foods high in sodium see this post.
High Potassium Additives & Foods
Foods high in potassium need to be limited and possibly avoided during stage 5 kidney disease when potassium levels are high.
In fact, limiting potassium when it is not appropriate can increase the risk of worsening kidney function.
One area that may help control potassium levels in your blood is to avoid potassium additives as much as possible.
Potassium additives are used in processed foods to enhance flavor, preserve, and be used as a salt substitute.
These additives can be highly absorbed and therefore have an impact on blood levels.
Potassium from natural sources such as fruits and vegetables are not always as highly absorbed. These foods also come with other nutritional benefits such as fiber.
Fiber can help with bowel movements, which can also help remove potassium from the body.
Therefore, have a thorough conversation with your dietitian about your potassium needs before putting any severe potassium restriction in place.
If you do in fact need to limit high potassium foods, we will include high potassium food lists for you below. We will also link to other articles that cover potassium in different foods and food groups.
High Potassium Food Lists
Vegetables high in potassium include
- Artichokes
- Avocados
- Brussels sprouts
- Sweet potatoes
- Bamboo Shoots
- Broccoli
- Beets/beet greens
- Butternut Squash
- Kohlrabi
- White Mushrooms
- Okra
- Parsnips
- Potatoes
- Pumpkin
- Rutabagas
- Spinach
- Carrots
- Brussels Sprouts
- Chinese Cabbage
- Leafy greens (except Kale)
- Hubbard Squash
- Tomatoes/Tomato products
Dairy products high in potassium include
Fruits high in potassium include
- Apricot
- Banana
- Cantaloupe
- Dates
- Figs, raisins, and other dried fruits
- Honeydew
- Kiwi
- Mango
- Prunes/prune juice
- Nectarine
- Orange
- Papaya
- Pomegranate
Nuts and seeds high in potassium include
- Hemp seeds
- Pistachio
- Squash and pumpkin seeds
- Flax seeds
- Hazelnuts
- Almonds
- Brazil nuts
- Peanuts and peanut butter
- Sunflower seeds
- Pine nuts
- Chestnuts
- Cashews
- Coconut
Read more about potassium in nuts here.
Grains high in potassium include
- Bran/bran products
Beans and legumes high in potassium include
- Baked Beans
- Lentils
- Refried Beans
- Black beans
- Dried beans and peas
Beverages high in potassium include
- Vegetable Juices
- Coconut water
- Grapefruit juice
- Orange Juice
- Pomegranate Juice
In addition to the above groups, other foods high in potassium include
- Chocolate
- Molasses
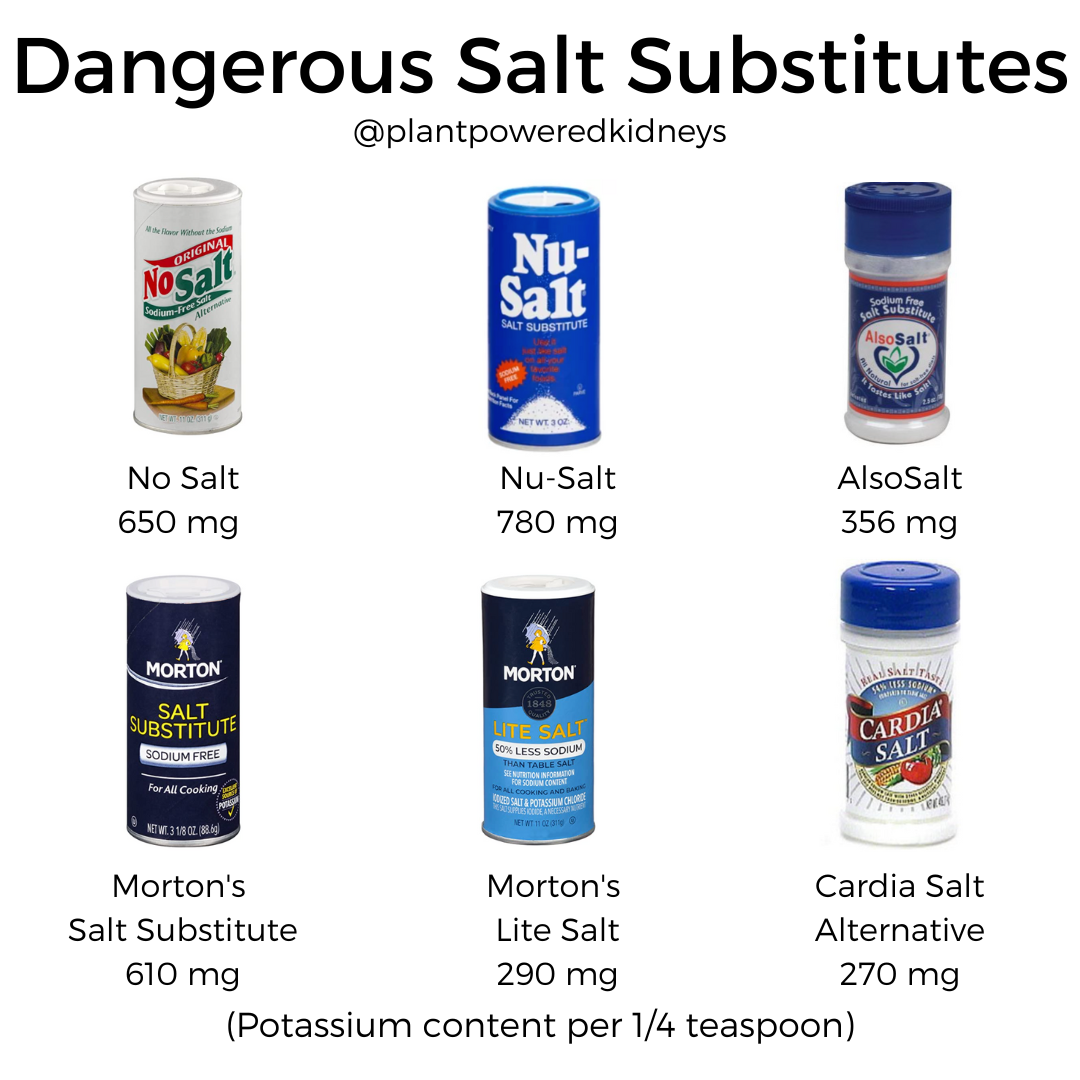
- Salt Substitutes
- Lite Salt
- Salt-Free Broth
- Snuff/Chewing Tobacco
A renal dietitian can help customize a diet that will meet your potassium needs.
High Phosphorus Foods
Often during stage 5 kidney disease, the kidneys cannot filter phosphorus and it needs to be limited in the diet.
The type of phosphorus will be important when it comes to making the biggest difference in your diet.
Inorganic phosphorus is a type of phosphorus that is added to foods as a preservative. This type of phosphorus is also highly absorbed and can be harder to control.
Start by reviewing the ingredient lists of the food in your house. Look for any ingredient that includes the letters P-H-O-S.
Examples of inorganic phosphorus include;
- Dicalcium phosphate
- Disodium phosphate
- Monosodium phosphate
- Phosphoric acid
- Sodium hexameta-phosphate
- Trisodium phosphate
- Sodium tripolyphosphate
- Tetrasodium pyrophosphate
Avoiding these types of ingredients as much as possible can make a significant difference in phosphorus control in your diet.
Foods with inorganic phosphorus can be found in:
- Canned foods
- Soups
- Canned drinks
- Deli & Processed meats (examples: hot dogs, bacon, sausage)
- Cocoa & Chocolate drinks
- Dark colas & Pepper type soda (Dr. Pepper)
- Canned iced teas
- Candies
- Muffins/Pastries/baked goods
- Pizza
- Ready to eat foods
- Chips/crackers
- Cereals
- Non-dairy creamers
- Jarred sauces
- Puddings
- Energy drinks
- Flavored waters
- Lemonades
- Frozen and prepared meats (chicken nuggets, meal kits, etc)
- Processed cheeses
- Products containing aluminum phosphate (baking powder)
If you can guarantee that you are not consuming any inorganic phosphates, you may need to limit organic phosphorus as well.
Organic phosphorus is the type of phosphorus that is found naturally in foods.
These mostly include foods from beverages, dairy, protein, and grain food groups.
Foods with naturally organic phosphorus include
- Beer/ale
- Cheese (especially hard cheeses)
- Cocoa
- Dried beans
- Milk
- Nuts
- Peanut Butter
- Peas
- Chicken
- Turkey
- Pork
- Ham
- Fish
- Shellfish
- Game meats
- Whole eggs
- Yogurt
- Cottage Cheese
- Leavened bread
Working with a dietitian can help you gain more insight into what foods you may be eating that could contribute to high phosphorus levels.
Foods Fortified with Calcium
During stage 5 kidney disease, foods fortified with calcium will need to be eliminated from the diet if calcium levels are elevated.
Dairy foods like milk, cheese, yogurt, and ice cream are sources of calcium.
Dairy can also be a source of organic and inorganic phosphorus, as well as potassium. These may be other reasons dairy foods need to be limited or avoided.
Animal Proteins
Eating high amounts of animal protein when you have stage 5 kidney disease will cause metabolic acidosis.
Additionally, following a low protein diet can protect remaining kidney function.
To maintain your health you want to limit or avoid the following high animal proteins.
- Chicken
- Poultry
- Shellfish
- Beef
- Lamb
- Game meats
- Milk/dairy
- Eggs
If you have protein limitations you also should avoid eating too much tofu, legumes, and beans.
This is because these foods are very high in protein. Limiting these foods will also preserve kidney health.
If you need a low-protein diet your renal dietitian can give you ideas on how to meet your protein needs while still maintaining kidney health.
Some also choose to include ketoanalogues as part of their low protein diet protocol. Talk with your dietitian about incorporating ketoanalogues into your diet routine.
Unhealthy Fatty Foods
Saturated and trans fats are unhealthy fats that should be eliminated from the diet.
They are found following foods
- Fatty meats
- Full fat dairy
- Baked goods (cakes, cookies, pies)
- Fried foods
- Shortening
- Margarine
- Foods with “hydrogenated” oils
Alcohol
Alcohol and kidney disease are an explosive combination when done in excess.
Drinking too much damages kidney function, increases blood pressure, and leads to weight gain.
When it comes to stage 5 kidney disease, even just one drink may be harmful for your health.
Avoiding alcohol altogether might be the right call to preserve kidney function.
Foods to Include in a Stage 5 Chronic Kidney Disease Diet
Like other phases of CKD, there is also a specific stage 5 kidney disease diet that should be followed.
This kidney disease treatment diet includes
- Foods with low sodium
- Low potassium foods
- Low phosphorus foods
- Calcium foods that are low in phosphorus
- Adequate protein mainly from plant sources
- Complex carbs
- Healthy fat foods
We will also talk about food for dialysis patients that should be added to the diet.
Low Sodium Foods
Low sodium foods should be part of the low kidney function diet. It is necessary for preserving kidney health. It lowers blood pressure and the risk of cardiovascular disease.
Look for no and low-sodium foods. Some naturally contain little or no salt. Others are made as low and salt-free options.
Dry beans, fresh and dry herbs, whole grains, rice, fruit, and vegetables do not contain any sodium.
If you eat rice and pasta be sure to get ones with no added salt.
Frozen fruits and vegetables without added dressings or seasonings also are free of sodium.
Spices and herbs that are fresh have no salt. You can also get sodium-free dried versions of herbs and spices.
Snacks with no sodium include unsalted popcorn, unsalted pretzels, and unsalted tortilla or corn chips.
Vinegar and dry mustard are naturally sodium-free. If you use other salad dressings or sauces, it is best to make them yourself or buy only low sodium brands.
Fresh meat, eggs, poultry, fish, and natural cheeses don’t have any sodium. If you have deli meat make sure it is low in sodium unless you have a phosphorus restriction. In that case, it should be avoided completely.
Soup is ok if you make one with no sodium or you buy a low-sodium variety. The same goes for casseroles and canned foods.
Learn more about a low sodium diet here.
Low Potassium Foods
The stage 5 kidney disease diet plan should include plenty of low potassium foods.
There are many options of low potassium foods among fruits, vegetables, dairy, protein foods, grain, and beverages.
Low potassium vegetables include
- Asparagus
- Arugula
- Bamboo Shoots
- Broccoli
- Carrots
- Cauliflower
- Celery
- Collard Greens
- Cucumber
- Eggplant
- Green Beans
- Kale
- Lettuce
- Mustard Greens
- Onion
- Peas
- Peppers
- Radicchio
- Red Cabbage
- Scallions
- Summer Squash (like zucchini)
- Tomatillo
- Water Chestnuts
- White Mushrooms
Fruits that are low in potassium are
- Apples
- Applesauce
- Apricots
- Blueberries
- Cherries
- Cranberries
- Fruit Cocktail
- Grapes
- Lemon
- Lime
- Mandarin Orange
- Pear (Bosc)
- Pineapple
- Plum
- Raspberries
- Rhubarb
- Strawberries
- Tangerine
- Watermelon
Dairy products that are low in potassium are cottage cheese and eggs.
Protein foods low in potassium include pecans, seitan, walnuts, tofu, and tuna.
Grains low in potassium include barley, brown rice, buckwheat, bulgar, plain oatmeal, pasta, popcorn, teff, whole wheat bread, and wild rice.
Beverages low in potassium are apple juice, coconut milk, coffee, cranberry juice, ginger ale, grape juice, lemonade, oat milk, pineapple juice, rice milk, and brewed tea.
Despite these foods being low in potassium, eating too many of them can add up to a lot of this nutrient. So be sure to watch your serving sizes.
In addition, protein foods and beverages may need to be limited if you have protein or fluid restrictions. Check with your renal RD about how to get enough potassium without going overboard.
Get a full list of low potassium foods in this post.
Low Phosphorus Foods
Fruits, vegetables, and whole grains have low phosphorus amounts and are not considered a source of phosphorus in our diet.
Therefore, enjoy a variety of fruits and vegetables when it comes to following a low phosphorus diet.
Dairy foods low in phosphorus are vegan cheeses, sherbert, cottage cheese, popsicles, and greek yogurt.
Protein foods low in phosphorus consist of both animal and plant varieties. Chicken, turkey, fish, beef, veal, eggs, lamb, and pork are animal proteins with low phosphorus.
Plant proteins low in phosphorus are tofu, soybeans, tempeh edamame, nuts, seeds, beans, and legumes.
For a comprehensive guide to the low phosphorus diet, check out this post.
Beverages low in phosphorus include rice milk, almond milk, black coffee, brewed tea, fruit juices ginger ale, and some milks, soda, and teas.
Unsalted pretzels, unsalted popcorn, unsalted crackers, pound cake, and sugar cookies are snacks low in phosphorus.
Calcium-Rich Foods
In rare cases, a stage 5 kidney disease diet may require more calcium-rich foods.
Anyone with stage 5 kidney disease and bone loss or low vitamin D levels need to make sure they get enough calcium and discuss vitamin D supplements with their dietitian.
In many cases, low calcium levels are associated with high phosphorus levels. Therefore, following a low phosphorus diet may be the best way to improve calcium levels.
However, some kidney patients may need to increase intake of calcium-rich foods at the direction of their own renal dietitian.
The one thing to remember with calcium foods is you need to make sure they are also low in potassium (if needed) and phosphorus.
If you have a lot of nutrient restrictions calcium needs can be met by adding foods like kale, arugula, and tofu to the diet.
If you suffer from calcium-based kidney stones, adding enough calcium-rich foods can be an important part in preventing them from occurring again.
Adequate Protein from Plant Protein Sources
As discussed earlier, the consumption of animal protein can lead to metabolic acidosis. To avoid this we encourage you to get most of your protein from plant sources.
The benefits of a plant-based diet will also improve heart health. This diet will be high in grains, fruits, vegetables, and healthy fats (learn more about these below).
If you decide to go vegan or vegetarian that can also reduce your risk of metabolic acidosis.
Don’t feel like you can give up meat? Instead of going cold turkey, try to scale back how much you are using.
Learn how to stretch out your protein intake with these tips
- Slice meat thin and use it sparingly
- Use milk substitutes to fill up your soups, rice, and pasta dishes
- Don’t make meat the star of the show, move it to a side dish as a complement to vegetables
- Cut meat into small pieces and mix with a lot of vegetables
- Fill your plate with grains and veggies and just a little bit of meat
- Make a hearty salad and top with small pieces of egg or meat
- In a casserole increase the number of veggies and decrease the meat
- Use pasta and other low-protein foods in soups
- A small quantity of a strong cheese will enhance flavor
Ask your healthcare team about your protein needs and how to get adequate intake.
Whole Grains and Foods High In Fiber
Getting more fruits and vegetables can prevent the inflammation that leads to nerve and neurological damage.
Getting blood sugar levels in a good place will also help to combat neuropathy that is associated with diabetic CKD.
Increasing your fiber and fluid intake can also improve autonomic neuropathy.
Diets for kidney failure need to include complex carbohydrates and high fiber foods. As we discussed earlier, refined carbs do nothing but hurt the kidneys.
So it is important to eat enough fiber and complex carbohydrates.
This means more vegetables, fruits, and whole grains. These foods will lower blood sugar, blood pressure, and keep you full longer.
Aim for at minimum of 6 servings of whole grains a day.
Some examples of whole grains include
- Whole wheat pasta
- Brown or wild rice
- Barley
- Quinoa
- Millet
- Couscous
- Amaranth
For a more comprehensive list of what grains to add to the diet see this post.
If you have diabetes, aim for approximately 50% of your calories from carbohydrates.
So on a 2,000 calorie diet, you want to get about 1,000 calories from carb sources.
This is about 250 grams of carbohydrates since each carb has 4 calories per gram.
Sticking to the same amount of carbs at each meal is another way to keep your blood sugar stable.
Healthy Fat Foods
Fat is an essential nutrient. Unfortunately, all fat is not created equal.
This means you want to stick with only healthy fat foods. These include monounsaturated (MUFAs) and polyunsaturated (PUFAs).
These healthy fats will reduce cholesterol and heart disease risk. MUFAs can lower the “bad” LDL cholesterol.
PUFA’s are made up of omega-6 and omega-3 fats. These cannot be made by the body and must come from the diet.
Oils, nuts, seeds, avocado, low-sodium olives, and fish are foods that provide healthy fats and can be added to the stage 5 kidney disease diet.
Oils include olive oil, avocado oil, sesame oil, and flaxseed oils. Some healthy nuts and seeds are chia, hemp hearts, flax, walnuts, pecans, macadamia nuts, and peanut butter.
Mackerel, herring, and trout are fishes that provide healthy fat.
Some fats may also fall into the category of your dietary restrictions. So be sure to ask your renal dietitian about choosing good fats that will not make you sick.
Iron-Rich Foods
Anemia affects almost all stage 5 kidney disease patients. Therefore, it can be helpful to include iron-rich foods.
These consist of both plant and animal sources of iron such as;
- Beef
- Lentils
- Leafy greens
- Mushrooms
- Garbanzo beans
- Tofu
- Flaxseed
- Olives
- Quinoa
Be sure to eat iron-rich foods with vitamin C-containing food. Vitamin C will enhance iron absorption.
Foods rich in vitamin C are:
- Bell peppers
- Strawberries
- Broccoli
- Chili peppers
- Thyme
- Kale
- Citrus fruit
Cooking with cast iron pans can also give your body an iron boost.
Some foods will reduce your iron absorption.
So be sure to eat iron-rich foods at least a few hours apart from the following:
- Dairy
- Foods with tannins like coffee and tea
- Phytates (grains, legumes, nuts, seeds)
Iron supplements may be required in some cases. It is important to discuss with your doctor and dietitian prior to starting any supplements as they may be harmful if not required.
Stage 5 Renal Diet Menu Plan
The renal diet meal plan for stage 5 kidney disease can be easy once you have a blueprint for what to add to your diet.
Below is a sample renal diet menu that will help maintain kidney function even in the end-stage of renal disease.
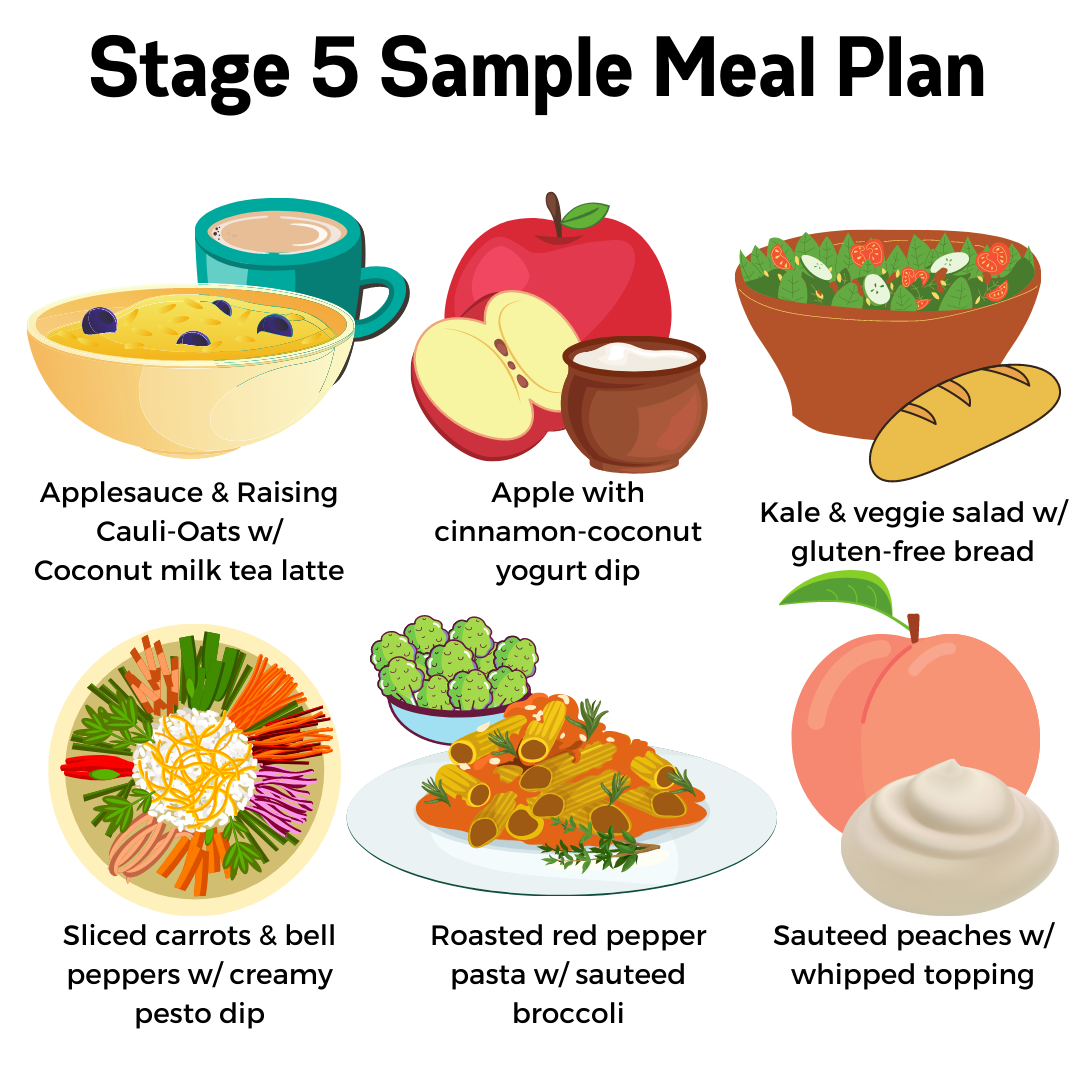
Breakfast: Applesauce & Raisin cauli-oats with a coconut milk tea latte
Snack: Apple with cinnamon-coconut yogurt dip
Lunch: Kale & veggie salad with gluten-free bread
Snack: Sliced carrots & bell peppers with creamy pesto dip
Dinner: Roasted Red Pepper Pasta with sauteed broccoli
Snack: Sauteed peaches with whipped topping
Our dietitians at Plant-Powered Kidneys have helped many people in stage 5 stay symptom-free and off of dialysis. You can click here to learn more about our team and work with us privately.
Renal Vitamins in Stage 5 Kidney Disease
Those with stage 5 kidney disease may have problems getting enough nutrients from their diet due to restrictions and limitations that are needed to maintain kidney health.
This gap in the diet should be filled with nutritional supplements and renal vitamins.
You may also need a special renal multivitamin.
They contain nutrients like:
- thiamin
- riboflavin
- pantothenic acid
- niacin
- pyridoxine
- cyanocobalamin
- folic acid
- biotin
- vitamin C
- vitamin D
- iron
- zinc
- selenium
- vitamin D
Examples of renal multivitamin supplements include
- Renavite ®
- ProRenal +D ®
- Nephrovite ®
- Dialyvite ®
Renal multivitamins give enough nutrition without any A, E, and K vitamins.
This is to avoid the large toxic doses that are found in regular over-the-counter multivitamins.
When Should You See A Renal Dietitian?
You should also work with a renal registered dietitian (RD). A renal dietitian knows all about renal nutrition.
They are responsible for helping to improve any nutrition issues that may arise from CKD.
A renal dietitian will put together an individualized plan that improves your nutrition status and helps protect and even improve your kidney function.
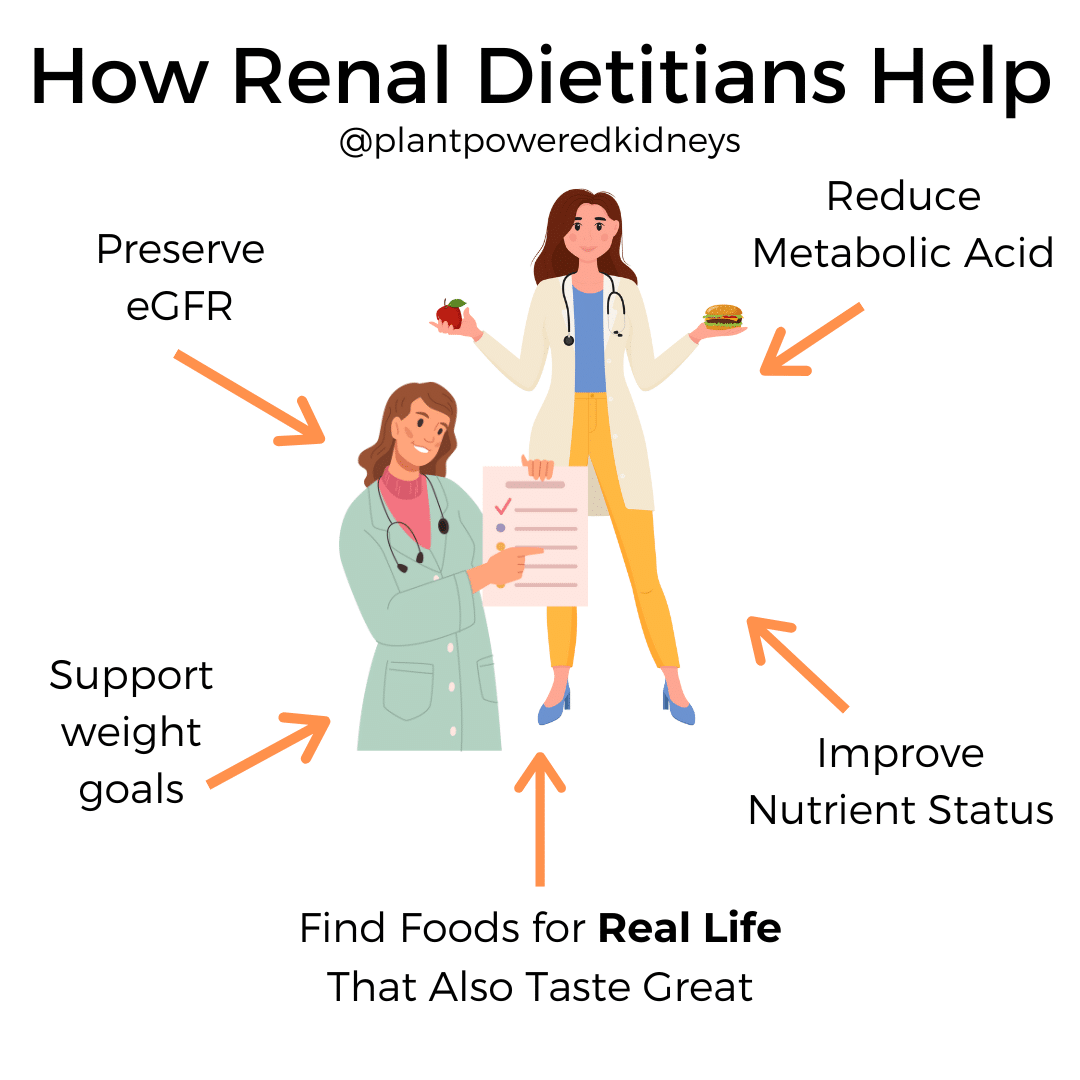
They can help you:
- Preserve eGFR
- Improve weight management
- Eat without limitations
- Understand your own nutritional needs and limitations
- Reduce metabolic acid
- Improve nutrient status
- Find foods for real life that also tastes great
- Help you move forward with CKD
If you don’t have a renal dietitian on your healthcare team, be sure to get one.
You can find a skilled renal dietitian by reaching out to your insurance company.
Alternatively, find a local dietitian in the National Kidney Foundations’ dietitian directory.
For anyone outside the states check out these international dietetic associations to find a renal dietitian in your own country.
Summary
Chronic kidney disease (CKD) is a serious issue that starts with slight damage to the kidneys. It can progress to stage 5 kidney disease. Known as end-stage kidney disease, ESKD, is the last stage of this condition. Over 85% of kidney function is gone by this time.
Dialysis or a kidney transplant is discussed at this time as an option for alleviating symptoms of end-stage kidney failure. Dialysis or transplant can help when significant symptoms occur and cannot be managed with diet, medications, and lifestyle changes. While this phase of CKD seems bleak there is still the ability to preserve even the minimal kidney function that remains.
Many people with stage 5 kidney disease choose to stay off of dialysis by following a low protein diet and using ketoanalogues. Working with a renal dietitian can be extremely helpful in providing specific diet guidelines and supplement support.
The way to do this is through managing underlying conditions like heart disease, diabetes, and imbalanced nutrient levels.
While medical interventions are important, nutrition and lifestyle changes seem to have the biggest impact on improving quality of life even during stage 5 kidney disease. Incorporating the help of a renal dietitian can improve nutritional status and prevent further kidney damage.

hi, it say’s in this article that ACE, ARBS and BETA BLOCKERS don’t excrete potassium so it causes potassium serum to rise? how about CALCIUM CHANNEL BLOCKERS? or any suggestions if there are any blood pressure lowering meds to replace this? thank you for the response.
Sean
Hi Sean, Calcium channel blockers don’t have an effect on potassium, but they may cause higher glucose levels. Medication recommendations would need to come from a physician. I hope this helps! 💚
I have just discovered I have serious kidney problem when was so weak I could walk back to car at the store I also have lost 50lbs from 190 lbs since the first symptoms I havent herd much about this. I started to research my health and soon could tell it was my kidneys so I quickly took control of my diet But I am so confused by the diet restrictions and cant apply any of them yet I need to see a renal dietitian soon but there are many in every health field that are not good they may have the credentials but will they give me good care ? thank you for this web sight I am very confused but also have less afraid and encouraged
Wow, I’m sorry to hear about your kidney problems! Seeing a dietitian is definitely the best way to accurately understand and personalize your own diet needs. There’s no longer a “one-size-fits-all” renal diet. A renal diet is now based on individual needs and preferences, besides medical history and kidney disease stage and cause. Here’s a link to find a dietitian that may help. 💚